Bronchospasm Emergency Preparedness Checklist
List your personal triggers below:
Check your emergency kit items:
Identify early warning signs:
- Increasing wheeze or whistling sound when breathing out
- Chest tightness
- Persistent cough, especially at night
- Difficulty speaking full sentences
- Feeling unusually anxious or restless
Call 000 (Australia) if you notice:
- Symptoms persist after 2–3 rescue inhaler doses
- Speech becomes slurred or unintelligible
- Blue tint around lips or fingernails (cyanosis)
- Chest pain or extreme fatigue
- Loss of consciousness or severe drowsiness
Your personalized action plan should include:
Imagine your lungs tightening in minutes, breath becoming shallow, and panic setting in. That’s a bronchospasm emergency - a life‑threatening situation that can strike anyone with asthma, COPD, or even a severe allergic reaction. Knowing exactly what to do before the crisis hits can turn a potentially fatal episode into a manageable event.
What Is Bronchospasm?
Bronchospasm is a sudden constriction of the airway muscles, leading to narrowed airways and reduced airflow. It commonly occurs in people with chronic respiratory conditions such as asthma or COPD. Triggers include viral infections, cold air, strong odors, exercise, and stress. The result is wheezing, coughing, and a frightening sense of suffocation.
Spotting the Early Warning Signs
Rapid recognition gives you the biggest advantage. Look for these cues before full‑blown breathlessness sets in:
- Increasing wheeze or whistling sound when breathing out.
- Chest tightness that feels like a band around the ribcage.
- Persistent cough, especially at night.
- Difficulty speaking full sentences.
- Feeling unusually anxious or restless.
If any of these appear, treat the episode as a potential emergency and move to the next steps immediately.
Build a Personalized Emergency Action Plan
Every person’s triggers and medication response differ, so a one‑size‑fits‑all plan won’t cut it. Your plan should include:
- Identify personal triggers. Write them down - pollen, pet dander, smoke, etc.
- List rescue medications. Include the name, dosage, and device (e.g., short‑acting beta‑agonist (SABA) inhaler).
- Specify dosing schedule. For a severe episode, many guidelines advise 2‑puffs every 20 minutes for the first hour.
- Provide emergency contacts. Include local ambulance number (in Australia, 000), your primary care physician, and a nearby hospital.
- Assign roles. If you’re not alone, decide who will fetch medication, who will call EMS, and who will keep you calm.
Print the plan, laminate it, and keep a copy in every high‑risk location - at home, work, school, and in your bag.
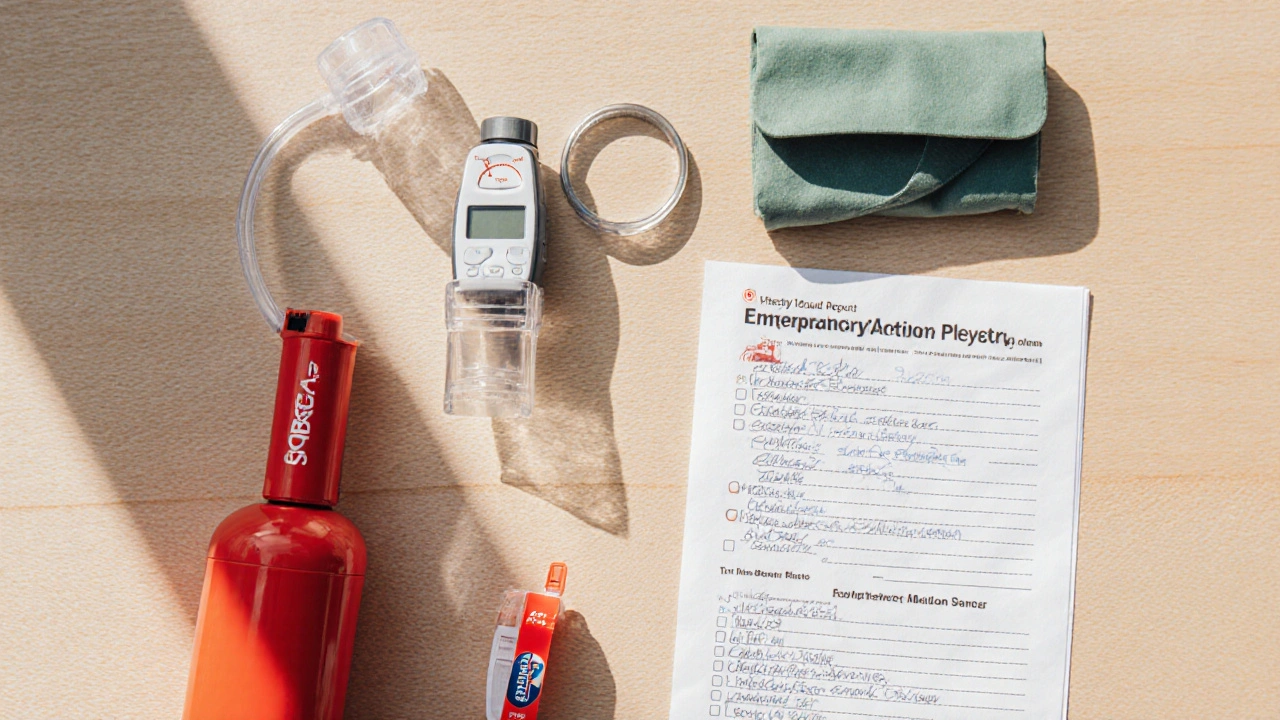
Gather Essential Supplies
When a bronchospasm strikes, you’ll have seconds to locate your items. Keep a dedicated "respiratory emergency kit" that contains:
- Rescue inhaler (SABA) - check expiration dates monthly.
- Spacer device - improves drug delivery, especially for children and older adults.
- Peak flow meter - helps you quantify airway obstruction.
- Portable oxygen cylinder (if prescribed) and appropriate mask or nasal cannula.
- Copy of your Emergency Action Plan.
- List of current medications and dosages.
- Medical alert bracelet or card mentioning bronchospasm risk.
Store the kit in an easily accessible drawer or cupboard, not inside a locked cabinet.
Master the Correct Inhaler Technique
Even the most potent bronchodilator won’t help if it never reaches the lungs. Follow these steps for a metered‑dose inhaler (MDI) with a spacer:
- Shake the inhaler for 5 seconds.
- Remove the cap and attach the spacer.
- Exhale fully, then place the mouthpiece in the spacer.
- Press the inhaler once while beginning a slow, steady inhalation through the mouth.
- Continue breathing in for 3-5 seconds, then hold the breath for 10 seconds.
- Remove the spacer, exhale gently, and repeat if another puff is needed.
Practice with a placebo inhaler weekly to keep the skill sharp.
Train Household Members and Caregivers
In a crisis, you may not be able to act on your own. Make sure someone else knows how to:
- Locate the emergency kit.
- Administer the correct number of inhaler puffs.
- Recognize when to call ambulance (e.g., no improvement after 3 doses).
- Perform basic first‑aid measures like positioning the person upright.
Run a mock drill every three months - simulate a bronchospasm, have a partner follow the plan, and time the response. This builds confidence and reduces hesitation.

When to Call Emergency Services
Even with fast‑acting medication, some episodes won’t calm down. Call ambulance if you notice any of the following:
- Symptoms persist after 2-3 rescue inhaler doses.
- Speech becomes slurred or unintelligible.
- Blue tint around lips or fingernails (cyanosis).
- Chest pain or extreme fatigue.
- Loss of consciousness or severe drowsiness.
When you dial 000, stay on the line, describe the situation, mention that the person has a known bronchospasm risk, and follow any instructions the dispatcher gives.
Preventive Strategies to Reduce Future Crises
Preparation isn’t just about reacting - it’s also about lowering the odds of an episode:
- Maintain regular follow‑up appointments with your respiratory specialist.
- Adhere to controller medications (e.g., inhaled corticosteroids) even when you feel fine.
- Use a peak flow meter daily to spot trends early.
- Avoid known triggers; keep windows closed during high pollen days, use HEPA filters, and stay away from smoke.
- Stay current on vaccinations (flu, COVID‑19, pneumococcal) that can precipitate attacks.
- Engage in a tailored pulmonary rehabilitation program to improve lung capacity.
Quick‑Reference Comparison of Common Rescue Inhalers
| Medication | Class | Typical Dose | Onset (minutes) | Duration (hours) |
|---|---|---|---|---|
| Albuterol (Ventolin, ProAir) | SABA | 90‑150µg per puff (1‑2 puffs) | 5‑10 | 4‑6 |
| Levalbuterol (Xopenex) | SABA | 45µg per puff (1‑2 puffs) | 5‑10 | 4‑6 |
| Ipratropium (Atrovent) | Short‑acting anticholinergic | 18‑36µg per puff (1‑2 puffs) | 15‑30 | 6‑8 |
Frequently Asked Questions
What’s the difference between a bronchospasm and an asthma attack?
A bronchospasm is the mechanical tightening of airway muscles, which is the core event in an asthma attack. In practice, the terms are often used interchangeably, but “bronchospasm” emphasizes the sudden muscle constriction, while “asthma attack” includes the broader inflammatory response.
Can I use a nebulizer instead of an inhaler during an emergency?
Yes, a nebulizer can deliver medication faster to the lungs, especially for young children or people who have difficulty using an MDI. Keep a portable jet nebulizer in your kit if you’ve been prescribed one, but remember it requires a power source and takes longer to set up than a quick‑relief inhaler.
When should I consider adding a long‑acting bronchodilator to my routine?
If you experience symptoms more than twice a week despite using a rescue inhaler, or your peak flow readings show a consistent decline, discuss adding a LABA (long‑acting beta‑agonist) combined with an inhaled corticosteroid with your doctor.
Do I need to carry a rescue inhaler if I’m hospitalized?
Hospitals typically have rescue meds on hand, but having your own inhaler ensures you receive the exact formulation and dose you’re accustomed to. Keep it in a small, labeled pouch on your person.
How often should I replace the inhaler and spacer?
Inhalers usually expire after 12‑18 months of use; check the printed expiry date. Replace the spacer every 6‑12 months or sooner if it becomes cracked, discolored, or difficult to clean.
Preparing for a bronchospasm emergency isn’t a one‑time checklist; it’s a habit you build over weeks and months. By understanding the condition, mastering medication technique, and having a clear action plan, you give yourself the best chance to stay safe when the airway suddenly tightens.





Jessica Wheeler
6 October, 2025 . 15:50 PM
It is a moral imperative that every individual with a respiratory condition treats preparedness as a sacred duty, not a optional afterthought. The checklist presented in the guide is thorough, yet many people ignore it out of sheer complacency. Ignoring the early warning signs is tantamount to flirting with disaster, and that carelessness cannot be excused. When you fail to maintain your inhaler, you are essentially holding a ticking time bomb in your pocket. The guide wisely stresses monthly inhaler checks, but the onus is on you to act responsibly. A rescue kit that is incomplete is as useless as a fire extinguisher with no powder. The inclusion of a portable oxygen cylinder is a lifesaving measure that should never be omitted. Its presence signals forethought, whereas its absence screams negligence. People who dismiss the need for a medical alert bracelet are ignoring simple, proven ways to get help faster. Every ounce of effort you invest in training caregivers pays dividends when a crisis hits. Practicing inhaler technique weekly is not just a suggestion; it is a non‑negotiable ritual for safety. If you cannot dedicate five minutes to a mock drill, you are betraying your own well‑being. The guide’s emphasis on a written action plan reflects a deep understanding of human psychology – people act faster when they have clear directives. Laminating that plan protects it from wear and tear, ensuring readability when you need it most. Moreover, keeping the plan in multiple locations mitigates the risk of misplacement; redundancy is a cornerstone of effective emergency preparedness. The article’s final reminder that preparation is a habit, not a one‑time checklist, should resonate with anyone who truly cares about their health. In short, neglecting any of these steps is not just careless – it is ethically indefensible.
Mikayla Blum
12 October, 2025 . 10:43 AM
Reflecting on the guide, I see a deeper lesson about mastering the present moment. Our breath is both a physical and philosophical anchor; when it narrows, our sense of control evaporates. By internalizing the step‑by‑step plan, we cultivate a calm mind that can act without panic. It's almost meditative, the way you rehearse the kit location and inhaler technique. Keep this ritual, and you'll find yourself less rattled when the unexpected arrives.
Jo D
18 October, 2025 . 05:37 AM
Oh great, another "essential" checklist – because we all love more paperwork before we can gasp for air. The jargon about "peak flow" and "spacer devices" feels like an over‑engineered circus for people who already struggle to remember where they left their inhaler.
Sinead McArdle
24 October, 2025 . 00:30 AM
I appreciate the thoroughness of the points made earlier, especially the emphasis on early detection. Maintaining a clear line of communication with caregivers is vital. It also helps to keep the emergency kit in a predictable spot to avoid confusion.
Katherine Krucker Merkle
29 October, 2025 . 18:23 PM
This guide hits the sweet spot between detail and readability. I especially like the suggestion to print and laminate the action plan – that way it survives kitchen spills. Adding a quick visual cue on the fridge could make it even more accessible. Also, marking the inhaler with a bright sticker helps everyone spot it faster. Overall, a solid resource for anyone wanting to be prepared.
Mark Quintana
4 November, 2025 . 13:17 PM
Good point about the laminated plan – bright stickers are a simple hack that works wonders. Keeping the kit in a clear container also speeds up retrieval. It's also smart to rotate inhalers before they expire, so you never run out unexpectedly.
Brandon Cassidy
10 November, 2025 . 08:10 AM
Building on what's been said, I think involving a trusted friend in the mock drills adds another layer of safety. When someone else practices with you, they internalize the steps too, which can be crucial if you're unable to act. Also, syncing the emergency contact list with your phone ensures you can call quickly even under stress. It's all about redundancy and shared responsibility.
Taylor Yokum
16 November, 2025 . 03:03 AM
When you think about a bronchospasm, picture it as a sudden roadblock on the highway of breath. The first thing you need is a clear detour map – that’s your emergency action plan. It should lay out who grabs the inhaler, who calls for help, and where the oxygen tank sits, all in a language anyone can follow. Next, the kit itself is your toolbox. A rescue inhaler is the primary instrument, but a spacer acts like a funnel, ensuring the medicine reaches deep into the lungs rather than bouncing off the mouth. A peak flow meter serves as a gauge; when numbers dip, you know the blockage is worsening and faster action is needed. Portable oxygen, if prescribed, is the backup generator that keeps the lights on while repairs are underway.
Now, imagine practicing this set‑up every week. It becomes second nature, like brushing your teeth. In a crisis, you won’t waste seconds hunting for items – you’ll grab the ready‑made pack and follow the steps you rehearsed.
The psychological side matters too. Knowing you’ve prepared reduces panic, which in turn keeps your airway muscles from tightening further. Staying upright, speaking calmly, and using slow breathing techniques are simple tricks that buy you precious time.
Finally, keep the plan visible. Tape a copy to the fridge, stick one inside the car’s glove compartment, and store one in your bag. Multiple copies mean the plan is always within arm’s reach, no matter where you are. By treating these steps as habits rather than a one‑off checklist, you turn a potential emergency into a manageable event, preserving health and peace of mind.
Taryn Esses
21 November, 2025 . 21:57 PM
Great checklist.
Albert Lopez
27 November, 2025 . 16:50 PM
One must commend the authors for assembling a compendium that borders on the encyclopedic, yet the presentation suffers from a certain pedantic excess. While the inclusion of dosage tables is undeniably useful, the superfluous repetition of basic definitions borders on the didactic. The reader is inundated with verbose prose that obscures the practical essence of emergency preparedness. Moreover, the insistence on laminate copies appears as an affectation rather than an evidence‑based recommendation. A more succinct, hierarchically structured protocol would serve clinicians and patients alike with greater efficiency. The psychological undertones-suggesting that preparation equates to moral superiority-introduce an unwarranted ethical dimension to what should remain a pragmatic guide. In summary, the document offers valuable content but is marred by an over‑infusion of editorial flourish, diminishing its utility.
Halle Redick
3 December, 2025 . 11:43 AM
Despite the heavy tone, the guide is a solid tool for staying safe. Keep the positivity flowing, and remember that every step you take now builds confidence for the future.
Erica Harrington
9 December, 2025 . 06:37 AM
Let's take this momentum and turn preparation into a daily habit. Even a quick glance at your emergency kit each morning can keep you ready. Encourage your family to join the practice – shared responsibility powers up safety. Remember, consistency beats occasional effort every time.