Ketoconazole Drug Interaction Checker
Check Your Medications
Ketoconazole has significant drug interactions due to its potent inhibition of CYP3A4. Enter medications you're currently taking to check for potential interactions.
Ever wondered why some fungal infections just won’t quit? The drug ketoconazole often shows up in the conversation, but how much do you really know about it?
What is ketoconazole?
When you need a quick overview, think of Ketoconazole as a synthetic azole antifungal that blocks the enzyme lanosterol 14α‑demethylase, halting ergosterol production and weakening the fungal cell membrane. In plain English, it starves the fungus of a key building block, causing it to leak and die.
How does it compare to other azoles?
Ketoconazole belongs to the broader Azole class, which also includes Fluconazole and Itraconazole. Here’s a quick side‑by‑side look:
| Attribute | Ketoconazole | Fluconazole | Itraconazole |
|---|---|---|---|
| Formulations | Oral tablets, topical cream, shampoo | Oral tablets, IV | Oral solution, IV |
| Primary use | Dermatophyte skin infections, systemic candidiasis (limited) | Systemic candidiasis, cryptococcal meningitis | Invasive aspergillosis, histoplasmosis |
| Hepatotoxicity risk | Higher - FDA black‑box warning | Low to moderate | Moderate |
| Drug interaction potential | Strong CYP3A4 inhibitor | Weak CYP2C9 inhibitor | Moderate CYP3A4 inhibitor |
| Typical dose (systemic) | 200‑400 mg once daily | 100‑400 mg daily | 200‑400 mg twice daily |
When do doctors prescribe ketoconazole?
Ketoconazole shines in a few niche scenarios:
- Dermatophyte infections such as athlete’s foot, ringworm, and scalp seborrheic dermatitis - usually as a cream or shampoo.
- Systemic candidiasis when other azoles are ineffective or unavailable, though oral use is now limited to cases where benefits outweigh liver‑risk.
- Hormonal disorders like Cushing’s syndrome - high‑dose ketoconazole can suppress adrenal steroid synthesis.
For most internal fungal infections, clinicians now reach first for fluconazole or itraconazole because they carry a cleaner safety profile.
Dosage forms and typical regimens
The drug comes in three main formats:
- Oral tablets: 200 mg once daily for mild‑to‑moderate systemic infections; up to 400 mg twice daily for severe cases (used only under specialist supervision).
- Topical cream: 2 % strength applied twice daily to affected skin for 2‑4 weeks.
- Medicated shampoo: 2 % solution used twice weekly to control dandruff caused by Candida albicans or Malassezia species.
Because the oral version can strain the liver, the FDA now recommends it only when topical options fail or when the infection is life‑threatening.

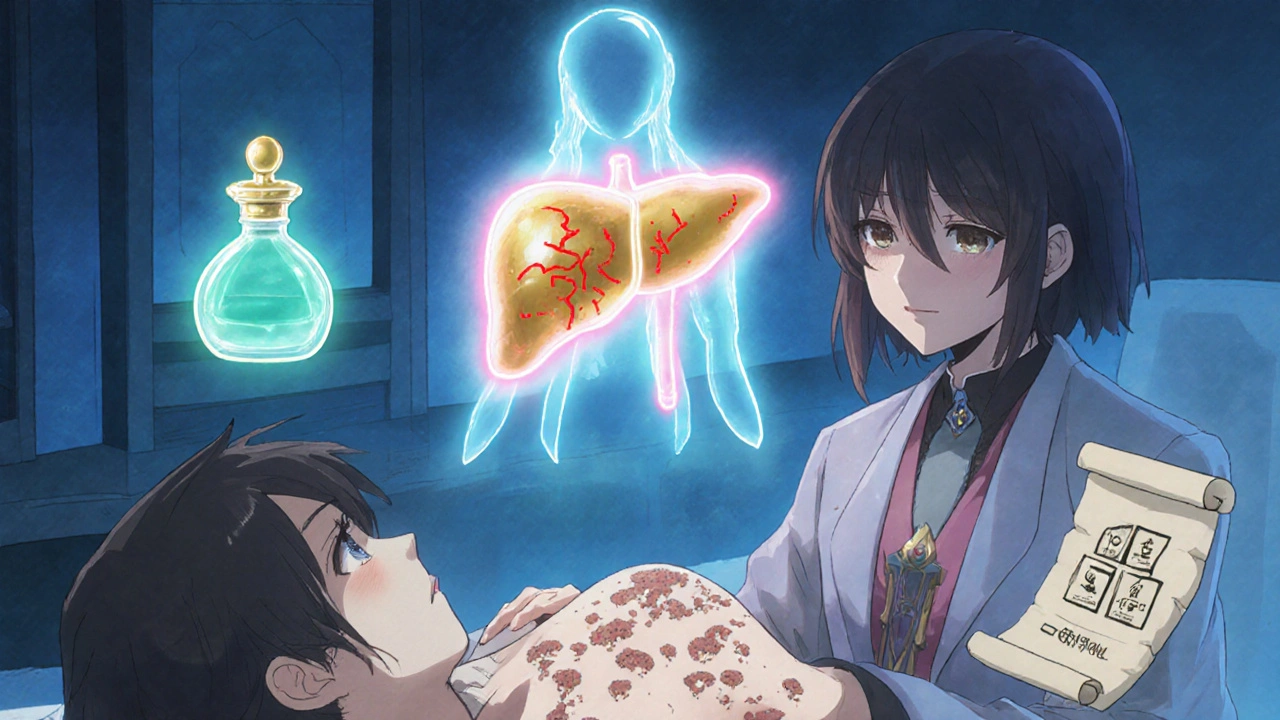
Safety profile - the liver warning
Back in 2013 the FDA added a black‑box warning for hepatotoxicity. Studies show an incidence of serious liver injury around 1 in 10,000 users, but the risk spikes with doses above 400 mg per day or treatment longer than two weeks.
Typical signs of liver trouble include:
- Yellowing of skin or eyes (jaundice)
- Dark urine and pale stools
- Unexplained fatigue or abdominal pain
If any of these appear, stop the drug immediately and get liver enzymes checked. Most clinicians will order baseline ALT/AST levels before starting oral ketoconazole and repeat them after one to two weeks.
Drug interactions you need to watch
Ketoconazole is a potent inhibitor of the cytochrome P450 3A4 enzyme (Drug interactions). This means it can raise blood levels of a long list of medicines, sometimes dangerously. Common culprits include:
- Statins (especially simvastatin) - risk of muscle breakdown.
- Calcium channel blockers - can cause low blood pressure.
- Oral contraceptives - may reduce effectiveness, so backup protection is advised.
- Immunosuppressants like cyclosporine - higher risk of kidney toxicity.
Always hand your pharmacist a full medication list before picking up ketoconazole.
Resistance and the future of ketoconazole
Fungal resistance is on the rise, especially among non‑albicans Candida species. Laboratory data from 2022‑2024 indicate that about 12 % of Candida isolates show reduced susceptibility to ketoconazole, largely due to mutations in the ERG11 gene that affect the drug’s target.
Because of this, researchers are exploring newer azoles (like isavuconazole) and non‑azole classes (echinocandins) for stubborn infections. Nevertheless, ketoconazole remains valuable for skin‑level diseases where resistance is less common.
Practical checklist for patients
Before you start a course, ask yourself these questions:
- Do I have a history of liver disease or elevated enzymes?
- Am I on any medication that the pharmacist warned could interact with ketoconazole?
- Is my infection confirmed as a dermatophyte or Candida species that responds well to ketoconazole?
- Do I have access to regular blood‑test monitoring if I’m taking oral tablets?
If you answer “yes” to any of the above, discuss alternatives with your doctor.
Frequently Asked Questions
Can I use ketoconazole shampoo for hair loss?
No. The shampoo is formulated to fight fungal scalp conditions, not to stimulate hair growth. Using it for hair loss hasn’t shown any benefit in clinical trials.
Is it safe to take ketoconazole while pregnant?
Ketoconazole is categorized as Pregnancy Category C. Animal studies showed some risk, and there aren’t enough human data. Doctors usually avoid oral ketoconazole during pregnancy unless the infection is life‑threatening.
How long does a typical skin infection treatment last?
For mild dermatophyte infections, a 2 % ketoconazole cream applied twice daily for 2-4 weeks usually clears the rash. Severe or widespread cases may need 4‑6 weeks.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and continue with your regular schedule - don’t double‑dose.
Can ketoconazole cause acne flare‑ups?
Rarely. Because it can alter skin flora, some people notice a temporary increase in acne when they start a topical regimen. The reaction usually settles within a week.
Bottom line
Ketoconazole still has a solid place in the antifungal toolbox, especially for skin‑level problems where its potency outweighs the liver concerns. Knowing when to choose it, how to dose it safely, and what to watch for can make the difference between a quick cure and a serious side‑effect.





Bobby Marie
19 October, 2025 . 21:10 PM
Check your liver enzymes before and during any oral ketoconazole course.
ashanti barrett
21 October, 2025 . 10:23 AM
If you’ve already got baseline labs, the next step is to keep an eye on any new fatigue, jaundice, or abdominal pain and call your doctor right away. The FDA’s black‑box warning exists for a reason, so repeat ALT/AST after one week and then bi‑weekly if you’re on a high dose. Many patients tolerate 200 mg daily without a hitch, but jump to 400 mg only under specialist supervision. In practice, I’ve seen clinicians pull the plug at the first sign of rising transaminases because the liver can’t afford a slow burn.
Leo Chan
22 October, 2025 . 23:53 PM
Hey folks, if you’re dealing with a stubborn ringworm, a two‑week course of 2 % ketoconazole cream can be a game‑changer. Apply it twice a day, massage it in, and you’ll usually see the rash start to fade within a few days. Keep the treatment going for the full four weeks even if it looks cleared – that’s how you stop the fungus from coming back. And don’t forget the shampoo for scalp issues; a couple of washes a week are enough to keep dandruff at bay.
jagdish soni
24 October, 2025 . 13:23 PM
One might argue that the very act of slathering a topical agent reflects a deeper epistemological surrender to pharmaceutical hegemony, yet the empirical data on ketoconazole’s ergosterol inhibition remain unassailable. The molecule’s lipophilicity ensures it penetrates the stratum corneum with minimal systemic spillover, thereby sidestepping the hepatic quandary that plagues its oral counterpart.
Latasha Becker
26 October, 2025 . 02:53 AM
Ketoconazole, a synthetic imidazole derivative, exerts fungistatic activity primarily through inhibition of the lanosterol 14α‑demethylase (CYP51) within the ergosterol biosynthetic cascade. This blockade precipitates accumulation of toxic methylated sterol intermediates that compromise membrane integrity. Pharmacokinetically, the oral formulation exhibits a bioavailability of approximately 50 % under fasting conditions, with a terminal half‑life ranging from 6 to 8 hours. Concomitant administration of high‑lipid meals can augment systemic exposure by up to 30 % via enhanced solubilization. Clinically, the drug maintains a minimum inhibitory concentration (MIC) of 0.125–0.5 µg/mL against most dermatophyte isolates, rendering it a first‑line topical agent. However, its systemic MIC against Candida spp. is often eclipsed by fluconazole, necessitating careful susceptibility testing. The hepatotoxic signal is mediated through reactive metabolite formation, which covalently modifies hepatic proteins and triggers immune‑mediated cytolysis. Incidence rates of grade 3–4 transaminase elevations approximate 0.02 % in large post‑marketing surveillance cohorts. Risk stratification algorithms incorporate baseline AST/ALT thresholds, concomitant CYP3A4 inhibitors, and genetic polymorphisms in CYP2C19. Drug–drug interaction potential is pronounced, given ketoconazole’s Ki value of <0.1 µM for CYP3A4, effectively converting it into a potent competitive inhibitor. Consequently, statins metabolized via CYP3A4, such as simvastatin, may experience plasma concentration surges exceeding 10‑fold. Regulatory guidance recommends dose reduction of the statin or substitution with a CYP3A4‑independent alternative. Emerging resistance mechanisms involve point mutations in the ERG11 gene, specifically Y132F and S405F, which diminish binding affinity. Molecular surveillance data from 2022‑2024 indicate a prevalence of these mutations in roughly 12 % of non‑albicans Candida isolates. Future therapeutic pipelines are exploring hybrid azole‑echinocandin conjugates to circumvent both resistance and hepatotoxicity. In summary, ketoconazole remains a valuable niche agent when deployed with rigorous monitoring, judicious dosing, and an awareness of its pharmacodynamic intricacies.
parth gajjar
27 October, 2025 . 15:23 PM
The tragedy of ignoring those molecular warnings is a saga repeated across clinics, where a patient’s liver becomes the sacrificial altar for a misguided prescription, and the drama unfolds in a cascade of bilirubin spikes that could have been averted with a simple lab check.
Maridel Frey
29 October, 2025 . 04:53 AM
It is prudent to document baseline hepatic panels prior to initiation, then schedule follow‑up tests at 7‑day intervals for the first two weeks, extending to bi‑weekly thereafter if the patient remains asymptomatic. Incorporating this protocol into the EMR order set ensures consistency across providers and mitigates the risk of missed elevations.
Madhav Dasari
30 October, 2025 . 18:23 PM
Yo, if you’re thinking about that fancy topical talk, just remember the cream’s magic is in staying on the skin, not in flooding your bloodstream. Keep it on the rash, rinse the shampoo after a few minutes, and you’ll dodge the liver drama entirely.