When your doctor orders a liver function test, it’s not because they think you have liver disease - not yet, anyway. It’s often a routine check, or maybe you’ve been feeling off, tired, or a little yellow. But what do those numbers on the lab report actually mean? ALT, AST, bilirubin - they sound like random letters and numbers. But they’re not. They’re clues. And if you know how to read them, you can understand what’s really going on inside your liver.
What Liver Function Tests Really Measure
The term "liver function tests" is misleading. These tests don’t measure how well your liver is working like a pump or a filter. Instead, they measure damage. When liver cells get injured, they leak enzymes into your blood. That’s what shows up on the test. The most common ones are ALT, AST, ALP, GGT, and bilirubin. Albumin and prothrombin time are also included - those are different. They measure what your liver can still make, not what it’s leaking.
ALT (alanine aminotransferase) is mostly found in the liver. If it’s high, it’s a strong sign that liver cells are damaged. AST (aspartate aminotransferase) is also in the liver, but it’s also in your heart, muscles, and kidneys. So if AST is up but ALT isn’t, something else might be going on - maybe a muscle injury or even a heart issue.
Bilirubin is a waste product your liver normally clears out. When it builds up, your skin and eyes turn yellow. That’s jaundice. Total bilirubin includes both unconjugated (old red blood cells breaking down) and conjugated (processed by the liver). If conjugated bilirubin is high, your liver or bile ducts are probably blocked.
Normal Ranges - And Why They’re Not Always Normal
Lab reports list normal ranges, but those numbers aren’t universal. For ALT, the typical range is 7-55 U/L. For AST, it’s 8-48 U/L. Bilirubin? Usually 3-17 μmol/L. But here’s the catch: these ranges vary by lab, sex, and body weight. Men tend to have higher normal ALT and AST levels than women. People with a BMI over 30 often have levels 10-15% higher than those with a healthy weight. That means a "normal" result for someone obese might still be abnormal for someone lean.
And here’s something most people don’t realize: up to 15% of healthy people have slightly elevated ALT or AST - no liver disease, no alcohol, no meds. If your ALT is 60 U/L and you feel fine, don’t panic. But if it’s 200 U/L? That’s a red flag.
ALT vs. AST: The Pattern That Tells the Story
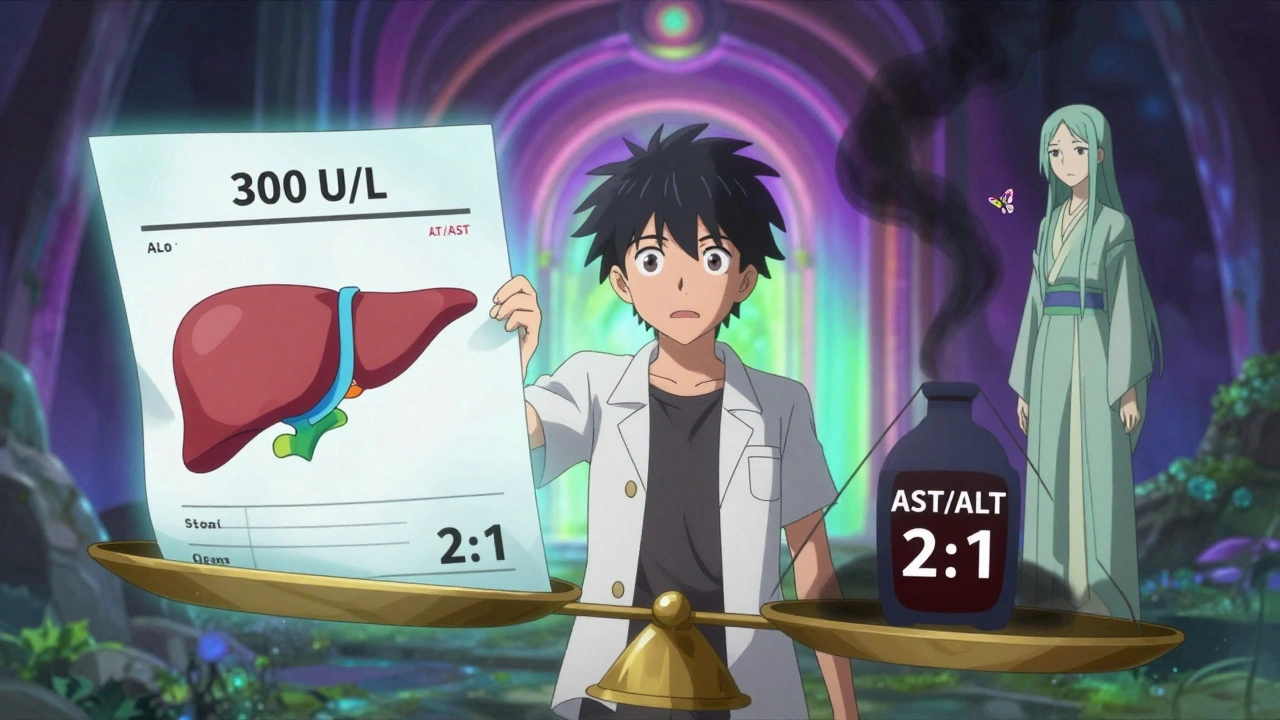
It’s not just about how high the numbers are - it’s about how they relate to each other.
If ALT is much higher than AST - say, ALT is 300 and AST is 100 - that’s classic for viral hepatitis, fatty liver disease, or drug damage. This is the most common pattern you’ll see.
But if AST is higher than ALT - especially if it’s twice as high - that’s a big clue for alcohol-related liver damage. An AST/ALT ratio above 2 is seen in about 90% of people with alcoholic hepatitis. That doesn’t mean you drink too much, but it’s a signal your doctor needs to ask about alcohol use.
There’s an exception: if AST is over 500 U/L, alcohol alone is unlikely to be the cause. Think acetaminophen overdose. That’s a medical emergency. In severe cases, ALT and AST can hit 1,000-2,000 U/L. That happens in acute viral hepatitis or massive liver injury from drugs or lack of blood flow.
And here’s a detail most don’t know: ALT sticks around longer than AST. Its half-life is about 47 hours. AST clears in about 24 hours. So if you had an injury a week ago, ALT might still be high while AST has already dropped. That’s why timing matters.
Bilirubin and ALP: When the Bile Flow Is Blocked
If ALT and AST are only mildly raised but bilirubin and ALP are sky-high, that’s a different story. This pattern is called cholestatic - meaning bile isn’t flowing properly. It could be a gallstone stuck in the bile duct, a tumor, or even a reaction to certain medications.
ALP (alkaline phosphatase) is found in the liver and bones. If ALP is high but GGT (gamma-glutamyl transferase) is normal, it’s more likely a bone issue - like a fracture or Paget’s disease - not liver disease. That’s why GGT is always checked with ALP. If both are up, it’s liver-related.
Isolated bilirubin elevation without high ALP or transaminases? That could be Gilbert’s syndrome - a harmless genetic condition where your liver processes bilirubin slowly. It’s common, often shows up in young adults, and gets worse with fasting or stress. No treatment needed.
Albumin and Prothrombin Time: The Real Liver Function Tests
Here’s where people get confused. ALT and AST show damage. But albumin and prothrombin time (PT) show whether your liver is still working.
Albumin is a protein your liver makes. If levels drop below 3.5 g/dL, it means your liver has been struggling for weeks or months. It takes 20 days for albumin to turn over. So a low albumin doesn’t mean you got sick yesterday - it means you’ve been sick for a while.
Prothrombin time measures how long it takes your blood to clot. Your liver makes clotting factors. If PT is prolonged, it’s a sign your liver isn’t making them anymore. This can happen fast - within days - after severe damage. It’s a warning sign of liver failure.
That’s why doctors don’t just look at ALT and AST. They look at the whole picture. A person with cirrhosis might have normal ALT and AST, but low albumin and high PT. That’s more dangerous than a high ALT with normal albumin.

When to Worry - And When to Wait
Not every elevated liver test needs a scan or a biopsy.
If your ALT is 50-100 U/L and you’re overweight, have type 2 diabetes, or drink alcohol occasionally, it’s likely non-alcoholic fatty liver disease (now called MASLD). The first step? Lose weight, cut sugar, get moving. Repeat the test in 3-6 months.
If your ALT is 200-500 U/L and you’re otherwise healthy, your doctor will check for hepatitis B and C, autoimmune liver disease, or medications. Many cases turn out to be harmless.
But if your ALT or AST is above 500 U/L - especially if it’s rising fast - that’s urgent. Same if bilirubin is over 50 μmol/L or you’re jaundiced. That’s when you need a specialist.
And here’s the truth: most primary care doctors overreact to mild elevations. One study found that 37% of patients with ALT between 41-80 U/L got unnecessary scans or referrals. If you’re asymptomatic and the rise is slow, watchful waiting is often better than rushing to action.
What’s Next? Beyond the Basic Tests
If your results are unclear, doctors now use more advanced tools. FIB-4 score combines your age, ALT, AST, and platelet count to estimate liver scarring. It’s free, fast, and surprisingly accurate. If it’s high, you might need an elastography scan - a painless ultrasound that measures liver stiffness.
New blood tests like the ELF test (enhanced liver fibrosis) are being used in clinics to detect early scarring before it shows up on imaging. These tests are especially helpful for people with fatty liver disease who don’t have symptoms but are at risk of cirrhosis.
And the guidelines are changing. The term "NAFLD" is being replaced with "MASLD" - metabolic dysfunction-associated steatotic liver disease. It’s not just about fat anymore. It’s about insulin resistance, high triglycerides, belly fat, and inflammation. That’s why lifestyle change is the only proven treatment.
Common Mistakes in Interpretation
People often blame the liver for everything. But ALT and AST can rise after intense exercise, a muscle injury, or even a heart attack. AST is especially tricky - it’s not liver-specific.
Another mistake: assuming normal ALT means a healthy liver. Someone with advanced cirrhosis can have normal transaminases. That’s why albumin and PT matter.
And don’t forget: some medications - even over-the-counter ones - can raise liver enzymes. Painkillers like acetaminophen, statins, antibiotics, and herbal supplements like green tea extract or kava can all cause temporary spikes.
The key? Look at the pattern. Look at the numbers over time. Look at your symptoms. Look at your weight, your alcohol intake, your meds. One number alone doesn’t tell the story.
Liver tests are not a diagnosis. They’re a starting point. And the best way to protect your liver? Eat real food, move every day, avoid excess alcohol, and don’t take more pills than you need. Your liver doesn’t need fancy treatments. It just needs you to stop hurting it.






Neelam Kumari
10 December, 2025 . 21:29 PM
Oh great, another ‘liver test explained’ post that makes me feel like my body is a science experiment gone wrong. I got my ALT at 62 last month and my doctor just smiled and said ‘probably fat’. Like, thanks for the medical insight, Dr. Obvious. I didn’t need a 10-page essay to tell me I’m unhealthy-I just needed someone to say ‘lose weight’ without the jargon. Also, why do labs have different ranges? Is my liver just bad at following rules?
Queenie Chan
11 December, 2025 . 18:09 PM
God, I love how liver enzymes are like the emotional barometers of your internal organs-ALT screaming in the corner because you ate pizza at 2 a.m., AST chilling in the gym with your quads, and bilirubin just quietly judging your life choices. And don’t even get me started on GGT-like the sneaky sidekick who only shows up when the party’s already over. It’s not a test, it’s a soap opera written in biochemistry. I once had a ‘normal’ ALT but a GGT that looked like it had been through a war. Turns out? I’d been drinking kombucha like it was liquid oxygen. Turns out, fermented tea can be a sneaky liver whisperer.
Stephanie Maillet
13 December, 2025 . 09:32 AM
It’s fascinating, isn’t it?-how our bodies communicate in such quiet, cryptic ways… ALT, AST… they’re not just numbers, they’re echoes of our choices, our neglect, our sleepless nights, our stress, our unspoken grief… And yet, we reduce them to ranges, to charts, to ‘normal’ and ‘abnormal’… But what is normal? Is it the lab’s definition? Or is it the quiet hum of a liver that’s been working overtime since childhood, carrying the weight of sugar, of anxiety, of unprocessed trauma? I wonder… if we stopped measuring and started listening… would we heal differently?
David Palmer
15 December, 2025 . 01:41 AM
bro why is everyone so scared of a little liver number? i had mine at 80 and i just drank less beer for a week and it was fine. also, i think doctors are just trying to sell you scans. my cousin got a $2000 ultrasound for an ALT of 55. he didn’t even have a belly. just a guy who ate too many burritos. chill out.
Aileen Ferris
15 December, 2025 . 21:41 PM
ok but what if ur alt is high but u dont drink or eat sugar? maybe its the 5g of aspartame in ur diet coke? or the fact u sleep in front of the tv? or maybe ur liver is just… vibin? i read on a forum once that liver enzymes go up if u look at your phone too much. idk. but i think its all a scam. they just want you to buy the detox tea.
Nikki Smellie
16 December, 2025 . 03:49 AM
Have you considered that these liver tests are being manipulated by Big Pharma to push statins, supplements, and liver ‘cleanses’? The ‘normal’ ranges were adjusted in 2017 to increase the number of people classified as ‘at risk’-that’s when the pharmaceutical industry’s stock in liver meds jumped 40%. The WHO never approved these new ranges. And why is GGT always checked with ALP? Because they know the truth: bile ducts are being blocked by fluoride in the water. The CDC has known since 2014. They just don’t want you to know. Please, for your liver’s sake-stop drinking tap water. Use a reverse osmosis filter. And stop taking acetaminophen. Even one pill could be the trigger. I’ve seen the data. I’ve read the redacted files. Your liver is not your enemy. The system is.