When a child accidentally swallows too much medicine, it’s not just a scary moment-it’s a medical emergency. Kids don’t process drugs the same way adults do. Their bodies are smaller, their organs are still developing, and even a small extra dose can cause serious harm-or worse. You might think, “It was just one extra drop,” or “They looked fine after.” But with some medications, the worst symptoms don’t show up for hours. By then, it could be too late.
What Does a Medication Overdose Look Like in a Child?
The signs of an overdose depend on what the child took. But there are some red flags that should never be ignored, no matter how mild they seem.For opioids-like prescription painkillers or fentanyl-the body shuts down slowly. Look for: small, pinpoint pupils; a limp body; slow, shallow, or stopped breathing; gurgling or choking sounds; cold, clammy skin; and lips or fingernails turning blue or gray. A child might appear to be asleep but won’t wake up, even when you shake them or rub their sternum. This isn’t just drowsiness-it’s respiratory failure in progress.
Acetaminophen (Tylenol) is one of the most common causes of pediatric overdose. The scary part? The first symptoms-nausea, vomiting, belly pain-often don’t appear for 24 hours. By then, the liver is already being damaged. A child might seem fine, even happy, playing in the next room. But inside, their liver cells are dying. Without treatment within 8 hours, the chance of survival drops sharply. After 16 hours, it’s often too late for the antidote to work fully.
For stimulants-like ADHD meds such as Adderall or Ritalin-the body goes into overdrive. Signs include: rapid heartbeat, high blood pressure, extreme agitation, hallucinations, seizures, chest pain, or sudden confusion. A child might be hyperactive one minute and collapse the next. In rare cases, this can trigger a stroke or heart attack, even in young children.
Other common culprits include cough and cold medicines, which often contain antihistamines or decongestants. These can cause drowsiness, hallucinations, fast heartbeat, or seizures. Herbal supplements and vitamins aren’t safe either-iron overdose from children’s multivitamins can cause vomiting, bloody stools, and organ failure.
When to Call 911 vs. Poison Control
This is the most critical decision you’ll ever make in a medical emergency.Call 911 immediately if your child is:
- Unresponsive or can’t be woken up
- Not breathing or breathing very slowly
- Having seizures or uncontrollable shaking
- Showing signs of a severe allergic reaction-swollen lips, tongue, or face, or a spreading rash
- Blue or gray skin, especially around the lips or fingertips
These are life-threatening signs. Don’t wait. Don’t text. Don’t Google. Call 911 right away. If you have naloxone (Narcan) and suspect an opioid overdose, give it immediately. One dose, then wait 2-3 minutes. If there’s no improvement, give another. Keep giving doses until help arrives.
Call Poison Control (800-222-1222) if:
- You suspect your child took medicine but they show no symptoms yet
- You’re unsure how much they took
- You found an empty bottle or pill container but the child seems okay
- You’re worried about a possible overdose but don’t see life-threatening signs
Poison Control experts are trained to ask the right questions: What was taken? How much? When? How old is the child? They’ll tell you whether to watch, go to the ER, or just stay calm. They’ve handled millions of cases. They won’t judge you. They’ll help you act fast.
Don’t wait for symptoms to appear. With acetaminophen, you might have only a 6-8 hour window to save a child’s liver. With opioids, every minute counts. Poison Control can guide you through the next steps while you’re still in shock.
Why Waiting Is Dangerous
Many parents think, “They’re sleeping, not crying, so it’s probably fine.” That’s exactly when things get deadly.Acetaminophen overdose is silent. The liver doesn’t scream. It just stops working. By the time a child vomits or looks sick, the damage is already done. Studies show that giving the antidote, N-acetylcysteine (NAC), within 8 hours of ingestion is 100% effective. After 16 hours, it’s only 40% effective. That’s not a gamble you can afford.
Fentanyl is even more dangerous. It’s 50-100 times stronger than morphine. A tiny amount-smaller than a grain of salt-can kill a child. And it’s often mixed into other pills or powders without warning. If you find a pill you don’t recognize, don’t touch it. Call Poison Control. They can help you identify it.
Even if your child seems fine after taking something, don’t assume safety. Some drugs cause delayed reactions. A child might act normal for hours, then suddenly collapse. That’s why experts say: when in doubt, call Poison Control.

How Overdoses Happen-And How to Prevent Them
Most pediatric overdoses aren’t accidents. They’re preventable.One of the biggest causes? Double-dosing. Parents give Tylenol for fever, then give a cold medicine that also has acetaminophen. Two doses become four. A child ends up with a toxic amount. The CDC says 70% of acetaminophen overdoses in kids happen this way.
Another common mistake? Using kitchen spoons. Liquid medicine comes with a syringe or cup for a reason. A teaspoon is not a measuring spoon. A tablespoon is not a medicine cup. Even a half-milliliter error can be dangerous in a toddler.
And don’t forget: medications aren’t candy. Never say, “This will make you feel better, like candy.” Kids mimic what they hear. If medicine tastes sweet and you call it candy, they’ll think it’s okay to eat.
Here’s what actually works:
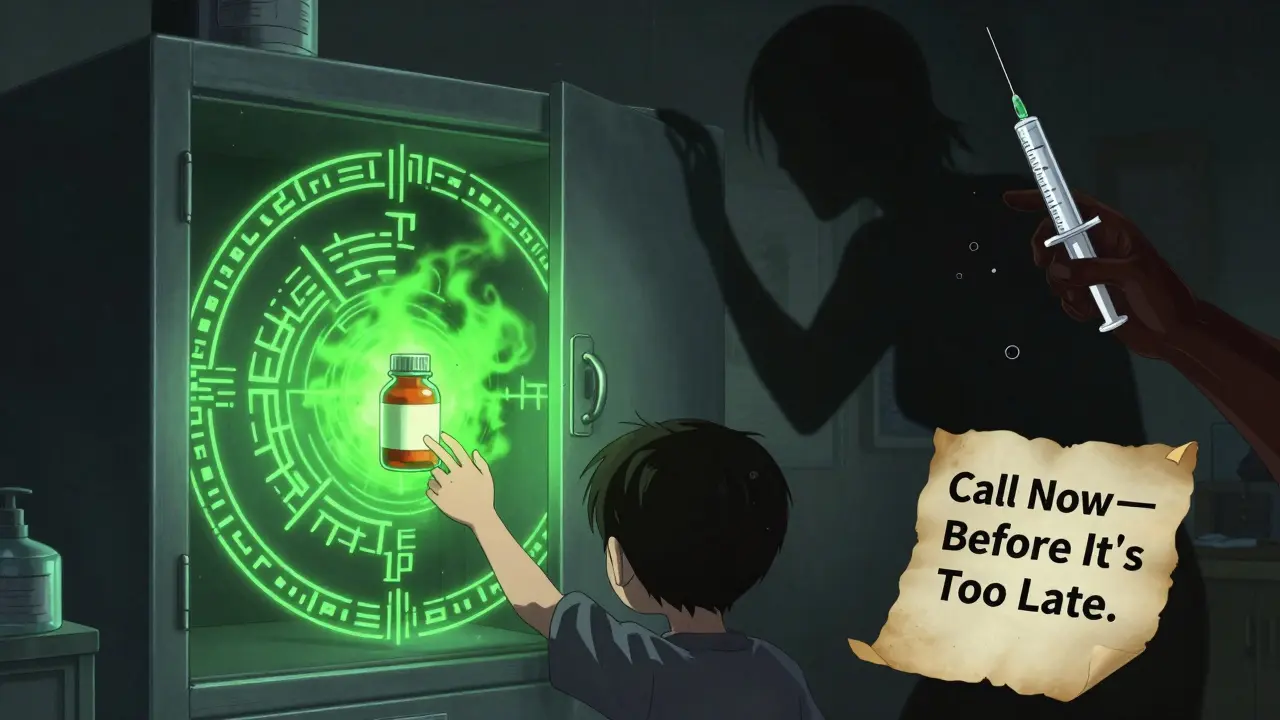
- Store all medications-prescription, OTC, vitamins-in a locked cabinet, out of sight and reach.
- Use child-resistant caps properly. (Yes, 20% of poisonings still happen even with them.)
- Keep meds in their original bottles. No more dumping pills into random containers.
- Always check the active ingredient. If two medicines say “acetaminophen,” don’t give both.
- Use the measuring tool that comes with the medicine. Never guess.
The FDA has started requiring clearer labeling and unit-dose packaging for liquid acetaminophen. Since 2020, this has cut accidental overdoses by 19%. But it’s not enough. You still have to be vigilant.
What to Do Right Now
If you think your child took too much medicine:- Don’t wait. Don’t watch. Don’t hope it’s fine.
- Call Poison Control. Dial 800-222-1222. It’s free, confidential, and available 24/7.
- If they’re unresponsive or not breathing, call 911 immediately. Start rescue breathing if you’re trained.
- If you have naloxone and suspect opioids, give it now. One dose. Wait. Give another if needed.
- Bring the medicine bottle. Even if it’s empty. The label tells the experts what’s inside.
Don’t try to make your child vomit. Don’t give milk or charcoal unless a professional tells you to. These old-school tips can make things worse.
What Happens After You Call
Poison Control will ask you a few quick questions:- What did the child take?
- How much?
- When?
- How old is the child?
- Are they showing any symptoms?
They’ll use a database of over 100,000 substances to assess risk. Then they’ll tell you:
- Watch at home
- Go to the ER
- Wait for EMS
They’ll even text you follow-up instructions. Many families don’t know that Poison Control now offers webPOISONCONTROL-a free online tool that gives instant guidance for non-emergency cases. You can use it while you’re on the phone or waiting for help.
And if you’re worried about a future incident? Talk to your pediatrician. Ask about safe storage, proper dosing, and what to keep on hand-like naloxone-if you’re caring for a child on opioids or in a home where others take prescription meds.
Final Thought: You’re Not Alone
Over 1 million pediatric medication exposures are reported to Poison Control every year. Most are accidental. Most are preventable. But every single one is a wake-up call.It’s not about blame. It’s about speed. The difference between calling Poison Control in 10 minutes versus waiting 2 hours could be the difference between a full recovery and a lifetime of liver damage.
Keep the Poison Control number saved in your phone. Put it on the fridge. Tell your babysitter. Teach your older kids: if something feels wrong, call immediately.
Your child’s life might depend on it.
What are the first signs of acetaminophen overdose in a child?
The first signs of acetaminophen overdose usually appear 24 hours after ingestion and include nausea, vomiting, stomach pain, and loss of appetite. But liver damage can begin within hours-even before symptoms show. A child may seem perfectly fine during this time, which is why calling Poison Control immediately after a suspected overdose is critical.
Can I wait to see if my child gets sick before calling Poison Control?
No. Waiting is dangerous. Many medications, especially acetaminophen and opioids, cause silent damage that doesn’t show symptoms right away. By the time your child looks sick, it may be too late for the best treatment. Poison Control can assess the risk and tell you whether to wait or go to the ER-even if your child seems fine.
Is it safe to give my child activated charcoal after a suspected overdose?
Never give activated charcoal without professional advice. It can be harmful if given incorrectly-especially if the child is drowsy or having trouble breathing. It’s not effective for all substances, and it can interfere with other treatments. Always call Poison Control first before trying any home remedy.
How do I know if my child’s medicine has acetaminophen in it?
Always check the “Active Ingredients” section on the label. Acetaminophen may also be listed as APAP. Many cold, flu, and pain medicines contain it-even if they’re labeled as “children’s cold medicine” or “fever reducer.” Never combine two medicines unless a doctor says it’s safe.
Should I keep naloxone at home if my child isn’t on opioids?
Yes-if you have any prescription opioids in your home, or if someone else (like a relative or visitor) brings them in. Fentanyl is often mixed into other pills without warning. Even if your child doesn’t take opioids, they could accidentally ingest a pill containing it. Naloxone is safe, easy to use, and can save a life in minutes.
What should I do if my child swallows a whole bottle of vitamins?
Call Poison Control immediately. While most children’s vitamins are low-risk, iron overdose from multivitamins can be deadly. Symptoms include vomiting, diarrhea, stomach pain, and drowsiness. If a child swallows more than 20 mg/kg of iron, they need urgent medical care. Don’t wait for symptoms-call right away.
For more information on safe medication storage and dosing, visit the American Academy of Pediatrics or the CDC’s Poison Prevention page. Prevention is always better than emergency care.






Josh Kenna
18 January, 2026 . 10:42 AM
my kid took half a tylenol last week and i panicked so hard i called poison control just to be safe-they laughed and said it was fine, but i still keep their number on speed dial. better safe than sorry, right?
Lewis Yeaple
19 January, 2026 . 10:33 AM
It is imperative to note that the physiological metabolism of pediatric patients differs significantly from that of adults due to hepatic enzyme immaturity and renal clearance inefficiencies. Consequently, pharmacokinetic parameters must be recalibrated for dosing protocols in children under twelve years of age.
Jake Rudin
19 January, 2026 . 23:25 PM
It’s fascinating-really-to consider how society treats medicine like candy, and then acts shocked when children treat it like candy… We’ve built a culture where everything is a quick fix, and we forget that biology doesn’t care about convenience… The liver doesn’t care if you meant well… It just… dies… quietly… and then we cry.
Phil Hillson
21 January, 2026 . 19:20 PM
so like… why are we even talking about this like it’s news? every parent who doesn’t lock up meds deserves to lose their kid. i mean really. what did you think was gonna happen? they’re not pets, they’re kids. stop being lazy
Erwin Kodiat
23 January, 2026 . 07:59 AM
My niece swallowed a whole bottle of gummy vitamins last year. She was fine, but we didn’t know that until we called Poison Control. They talked us through it like we weren’t total panicking idiots. Honestly? I think they should be on every phone. Like 911. Or Uber.
Valerie DeLoach
24 January, 2026 . 04:04 AM
I’m a pediatric nurse, and I’ve seen too many cases where parents waited because ‘they seemed fine.’ The silence of acetaminophen toxicity is terrifying-it doesn’t scream, it just stops. Please, if you’re reading this, store meds like you store guns. Locked. Out of reach. And never, ever, in a purse or on a nightstand.
Christi Steinbeck
24 January, 2026 . 20:08 PM
STOP WAITING. Seriously. I got called to a hospital at 3am because a mom thought her kid was just ‘sleeping it off’ after swallowing a handful of Adderall. He had a seizure. He’s okay now, but he’s on meds for life because she waited. Don’t be her. Call. Now. Even if you’re embarrassed.
Jacob Hill
25 January, 2026 . 02:43 AM
Can I just say-measuring spoons are the devil? I used to use them… until my cousin’s kid got a toxic dose because ‘a spoon is a spoon.’ Now I use the syringe. Every time. Even if it’s annoying. Worth it.
Jackson Doughart
26 January, 2026 . 15:57 PM
The emotional weight of this post is not lost on me. I have two young children, and the thought of a single misplaced pill altering their future is paralyzing. I have installed a biometric lock on my medicine cabinet. It cost me $80. It is the best investment I’ve ever made.
Tracy Howard
28 January, 2026 . 00:18 AM
USA really is a mess. In Canada we have strict childproof packaging laws, mandatory labeling in both languages, and public education campaigns. Here? You’re expected to Google your way out of a medical emergency. Pathetic.
Aman Kumar
28 January, 2026 . 20:16 PM
Let me be clear: the pharmaceutical-industrial complex has weaponized parental guilt. They sell you meds with deceptive labeling, then profit from your panic. The real villain isn’t the parent-it’s the FDA, the CDC, and the companies that profit from preventable tragedies.
Lydia H.
30 January, 2026 . 09:21 AM
I used to think ‘just keep it high up’ was enough. Then I found my 3-year-old with a half-eaten bottle of ibuprofen… behind the cereal box. Kids are tiny detectives. Lock it. Even if you think they can’t reach it. They can.
Astha Jain
1 February, 2026 . 05:28 AM
why do we even need poison control? just dont give kids medicine lol. if they sick then they sick. maybe they need to learn to be tough
Malikah Rajap
2 February, 2026 . 09:23 AM
Did you know that 87% of accidental overdoses happen in homes where someone else-like a grandparent or visitor-is caring for the child? It’s not about bad parenting. It’s about communication. Talk to your babysitters. Your in-laws. Your friends. Even if it’s awkward. This isn’t about blame-it’s about connection.
sujit paul
4 February, 2026 . 03:31 AM
Consider this: the entire system is engineered to normalize risk. The FDA approves formulations with ambiguous dosing instructions. The media promotes ‘natural remedies’ with no regulation. And now we are surprised when children die? This is not negligence-it is systemic failure. The solution? Abolish the medical-industrial complex and return to ancestral wisdom.
Josh Kenna
4 February, 2026 . 11:10 AM
someone above said ‘don’t wait’ and i’m like… yeah but what if you’re alone? scared? don’t know what to do? poison control doesn’t judge. i called crying once. they stayed on the line for 22 minutes while i drove to the ER. they’re angels in lab coats.