Steroid-Induced Psychosis Risk Calculator
Calculate Your Steroid Risk
This calculator estimates the risk of steroid-induced psychosis based on your current dose. Use this to inform clinical decision-making.
When a patient on high‑dose steroids suddenly starts hearing voices or believing bizarre things, the clock starts ticking. Steroid‑Induced Psychosis is a medication‑induced psychotic disorder that appears after exposure to corticosteroids. Rapid identification can mean the difference between a short, treatable episode and a dangerous crisis. Below you’ll find the step‑by‑step approach that emergency clinicians use to spot, assess, and calm these patients before they harm themselves or others.
Why Steroids Can Flip the Mind
Corticosteroids mimic the body’s natural cortisol, but they jam the hypothalamo‑pituitary‑adrenal (HPA) axis. By flooding glucocorticoid receptors and suppressing mineralocorticoid activity, they create an imbalance that messes with mood, cognition, and perception. The exact neurobiology is still a research focus, yet clinical data show a clear dose‑response curve: patients receiving >40 mg/day of prednisone develop psychiatric symptoms 4.6 % of the time, climbing to 18.4 % when the dose exceeds 80 mg/day.
Job 1 - Spot the Early Red Flags
In the first five days after starting a steroid, watch for:
- Confusion or “brain fog” that seems out of proportion to the illness.
- Restlessness, agitation, or inexplicable irritability.
- Rapid mood swings - euphoria that flips to despair in minutes.
- Early auditory hallucinations (hearing whispers or comments).
If any of these pop up, ask the patient when the steroid was started and at what dose. The timeline often aligns perfectly with the onset of symptoms.
Job 2 - Run a Focused Emergency Assessment
The goal is twofold: keep everyone safe and rule out medical mimics. A structured 4‑step protocol works well:
- Safety first: Use verbal de‑escalation, a calm tone, and a low‑stimulus environment. If agitation escalates, have IM olanzapine (5‑10 mg) or IM haloperidol (2‑5 mg) ready.
- Confirm steroid exposure: Document drug name, dose, route, and initiation date.
- Exclude other causes: Check glucose, electrolytes, calcium, thyroid panel, toxicology screen, and consider infection or head injury.
- Start treatment: Taper the steroid (if possible) and begin a low‑dose antipsychotic.
The DSM‑5 criteria for substance/medication‑induced psychotic disorder require that the psychosis cannot be better explained by a primary psychiatric disorder, delirium, or another medical condition. In practice, that means a quick labs panel and a brief neuro exam are non‑negotiable.
Job 3 - Adjust the Steroid Dose Wisely
When the psychosis is linked to steroids, the most effective move is to lower the dose. Evidence shows that dropping prednisone below 40 mg/day (or dexamethasone below 6 mg/day) leads to symptom resolution in over 90 % of cases. Tapering must be gradual enough to avoid adrenal insufficiency, especially if the patient has been on steroids for weeks.
Typical taper:
- Day 1‑3: Reduce by 20 % of the current dose.
- Day 4‑7: Another 20 % cut if no rebound inflammation.
- After day 7: Switch to the lowest effective dose for the underlying disease, then continue a slow taper over 2‑4 weeks.
If the underlying condition (e.g., severe asthma flare) demands high‑dose steroids, you’ll need to control the psychosis pharmacologically while keeping the steroid level as low as clinically possible.
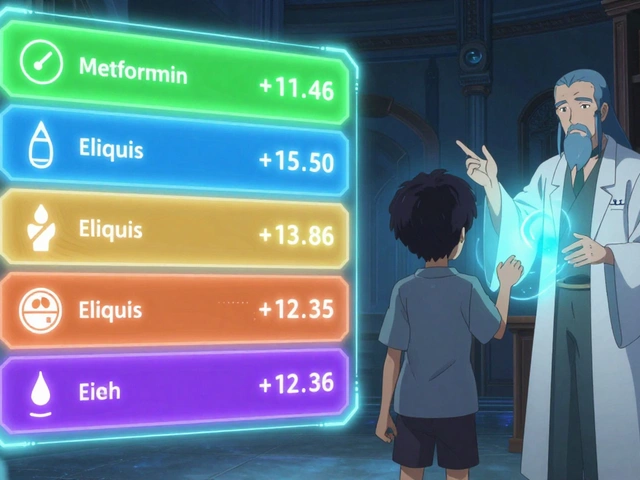
Job 4 - Choose the Right Antipsychotic
There is no FDA‑approved drug specifically for steroid‑induced psychosis, but several agents have solid real‑world data:
| Drug | Typical Dose (Oral) | Key Considerations |
|---|---|---|
| Olanzapine | 2.5‑20 mg/day | Effective for agitation; watch for metabolic side effects. |
| Risperidone | 1‑4 mg/day | Lower EPS risk; monitor prolactin. |
| Haloperidol | 0.5‑1 mg/day (oral) or 2‑5 mg IM | Fast calming; give benztropine or diphenhydramine to prevent EPS. |
| Lithium | 300‑600 mg BID (if no renal issues) | Prevents mania/psychosis recurrence; requires serum level checks. |
Start low, go slow. For most ED presentations, a single dose of oral olanzapine 5 mg plus a short‑acting benzodiazepine (lorazepam 1 mg) provides rapid calm without heavy sedation.
Job 5 - Coordinate Multidisciplinary Follow‑Up
Once the acute episode is under control, the patient needs a clear plan:
- Referral to liaison psychiatry for ongoing antipsychotic management.
- Education for the primary team on steroid‑related risks.
- Patient/family counseling about warning signs and when to call back.
- Document the episode in the electronic health record using the DSM‑5 code for medication‑induced psychotic disorder.
Studies show that when these steps are followed, long‑term psychiatric sequelae drop dramatically-most patients return to baseline within weeks.
Key Takeaways
- Steroid‑induced psychosis often appears within the first five days of high‑dose corticosteroid therapy.
- Early signs are confusion, agitation, and mood swings-treat them as red flags.
- Safety first: de‑escalate, then use low‑dose antipsychotics (olanzapine, risperidone, haloperidol).
- Lower the steroid dose below 40 mg prednisone (or equivalent) whenever possible.
- Arrange psychiatry follow‑up and educate the patient on warning signs.
Mini‑FAQ
How soon after starting steroids can psychosis appear?
Symptoms usually emerge within 1‑5 days, but rare cases have been reported up to two weeks after initiation.
Is a low dose of prednisone safe for patients with a history of psychosis?
Low doses (<20 mg/day) are generally well tolerated, yet clinicians should still monitor for mood changes, especially during dose adjustments.
What laboratory tests are essential in the ED?
Basic metabolic panel, glucose, calcium, thyroid‑stimulating hormone, urine toxicology, and a rapid infection screen (CBC, CRP) are recommended to rule out mimickers.
Can antipsychotics be stopped once the steroid is tapered?
Most patients can discontinue antipsychotics after symptoms resolve and the steroid dose is stable for at least one week, but a brief taper (3‑5 days) helps avoid rebound agitation.
Are there any preventive strategies for high‑risk patients?
Screen for personal or family history of mood disorders, use the lowest effective steroid dose, and consider prophylactic mood stabilizers like lithium under specialist supervision.
Being alert to the psychiatric side effects of steroids saves lives and prevents unnecessary suffering. The next time you see a patient on prednisone who suddenly sounds confused or terrified, remember the quick four‑step protocol above-you’ll be ready to act before the situation spirals.





Joe Langner
26 October, 2025 . 19:02 PM
Spotting the red flags early can feel like a light in a dark hallway – you just need to keep your eyes open. When a patient starts to mumble about hearing whispers after a burst of prednisone, it’s a cue to pause the dose and check labs. A quick check‑in with the nursing staff about the exact start date of steroids can shave minutes off the response time. Remember, even a small taper can tip the balance back toward stability, especially if the underlying disease is not flaring. Keep the conversation calm, use simple language, and let the patient know you’ve got their back, even if the meds got a little too wild.
Ben Dover
26 October, 2025 . 21:49 PM
The pathophysiological underpinnings of glucocorticoid‑induced psychosis warrant a nuanced appraisal of hypothalamic‑pitocentral feedback loops. Empirical data delineate a dose‑response relationship wherein prednisone exceeding 80 mg/day precipitates neuropsychiatric sequelae in upwards of 18 % of cohorts, a statistic that cannot be dismissed as stochastic variance. Consequently, a rigorous differential diagnosis must integrate serum cortisol quantification, electrolyte panels, and neuroimaging where indicated, to obviate conflation with primary psychotic disorders. Moreover, the therapeutic algorithm should prioritize tapering regimens consonant with adrenal axis preservation, supplemented by second‑generation antipsychotics with minimal extrapyramidal liability.
Tony Stolfa
27 October, 2025 . 00:35 AM
Look, Ben, you can drown us in jargon all you want, but on the floor we need a plan that works now, not a lecture on hypothalamic feedback. If a patient is screaming about voices, the fastest move is a 5 mg oral olanzapine and a controlled steroid taper, not a 30‑page differential. Your “rigorous differential” sounds nice on paper, but the ER doesn’t have time for endless panels unless the patient is unstable. So let’s cut the fluff and stick to what calms the patient in minutes.
Joy Dua
27 October, 2025 . 03:22 AM
When the mind is besieged by the synthetic surge of corticosteroids the very essence of perception is called into question
One must consider the delicate equilibrium of neurotransmitter cascades that are perturbed by excess glucocorticoid receptor activation
The resulting dysregulation manifests not merely as agitation but as a profound existential rupture in the patient’s reality
This phenomenon aligns with the ancient philosophical notion that external forces can unmoor the soul from its rational anchor
Clinically the hallmark is a rapid onset within days of initiating therapy, oftentimes accompanied by auditory aberrations that are misinterpreted as hallucinations
Laboratory assessment should be swift yet comprehensive, encompassing glucose, electrolytes, thyroid function and a basic toxicology screen
Neuroimaging is reserved for atypical presentations where focal lesions cannot be excluded
Therapeutic intervention must be twofold: attenuate the offending steroid dose and introduce a psychotropic agent with a favorable side‑effect profile
Olanzapine remains a frontline choice due to its sedative potency and relative metabolic tolerability in the acute setting
Risperidone offers an alternative when metabolic concerns predominate, though clinicians must monitor prolactin trajectories
Haloperidol provides rapid calm but necessitates anticholinergic co‑administration to mitigate extrapyramidal phenomena
Lithium, while not first‑line, can be contemplated in recurrent cases where mood stabilization is sought
The tapering schedule should respect adrenal recovery, typically reducing the dose by twenty percent increments over a week before further weaning
Multidisciplinary coordination ensures that psychiatry follow‑up is not an afterthought but an integral component of the care continuum
Finally, patient education on early warning signs empowers individuals to seek help before the crisis escalates
Holly Kress
27 October, 2025 . 06:09 AM
It’s useful to remind the whole team that steroid dose reduction should be individualized, especially when the underlying disease still demands anti‑inflammatory therapy. A gentle taper, combined with an antipsychotic at the lowest effective dose, often yields rapid symptom resolution without compromising disease control. Engaging the patient in the decision‑making process also helps reduce anxiety and fosters adherence to the follow‑up plan.
Chris L
27 October, 2025 . 08:55 AM
Great point about involving liaison psychiatry early; I’ve seen that a prompt referral can cut the length of stay by a day or more. Staying calm, using low‑stimulus environments, and keeping the steroid dose as low as the condition permits are all practical steps we can all adopt.
renee granados
27 October, 2025 . 11:42 AM
Look Chris you’re ignoring the fact that the pharma companies push high‑dose steroids to keep us hooked on their drugs and they never tell us about the brain side effects
Stephen Lenzovich
27 October, 2025 . 14:29 PM
Patriots don’t need foreign meds hijacking our minds.