PBM Spread Pricing: What It Is and How It Affects Your Medication Costs
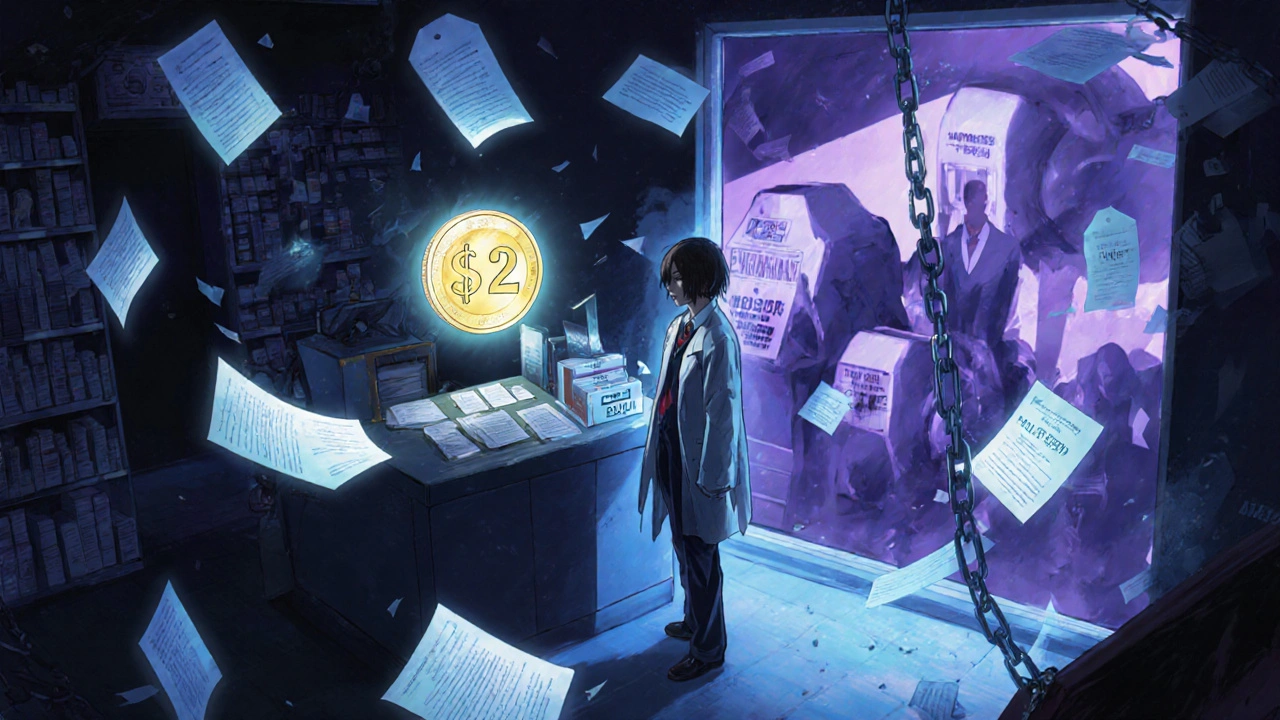
When you pick up a prescription, you might think the price you pay is what the pharmacy paid for the drug. But that’s not always true. Under PBM spread pricing, a practice where pharmacy benefit managers charge insurers more for a drug than they pay the pharmacy, keeping the difference as profit. Also known as price arbitrage, it’s a hidden layer in how prescription drugs are priced in the U.S. This isn’t about generic vs. brand-name drugs—it’s about who controls the money between the pharmacy, the insurer, and you.
PBM spread pricing directly impacts your out-of-pocket costs, especially if you’re on a high-deductible plan or pay cash. For example, a pharmacy might get $10 from the PBM for a $50 drug, but you’re charged $45 because the PBM tells your insurer the drug costs $45. The $35 difference? That’s the spread. It’s not disclosed. It’s not regulated. And it’s not your pharmacist’s choice. This practice is widespread across major PBMs like CVS Caremark, Express Scripts, and OptumRx. These companies act as middlemen between drug manufacturers, pharmacies, and health plans—but their profits often come from inflating prices you see at the counter.
It’s not just about big pharma. Even small independent pharmacies get squeezed. They’re forced to accept low reimbursement rates from PBMs just to stay in network, while patients get billed inflated prices. And because PBMs control formularies and pharmacy networks, you often don’t have a choice—you’re locked in. This system makes it harder to compare prices, understand true costs, or find affordable alternatives. It’s why two people with the same drug and same insurance can pay wildly different amounts.
What you’ll find in the posts below isn’t a list of drug comparisons or dosage guides. It’s the real-world fallout of systems like PBM spread pricing. You’ll see how drug pricing tricks affect adherence, why some medications suddenly cost more, and how people are fighting back with tools like the FDA database or generic alternatives. These aren’t abstract policy debates—they’re stories of people paying more because of hidden markups, trying to stretch their budgets, or wondering why their insulin price jumped again. The posts connect the dots between corporate pricing models and your daily health decisions. You’re not just reading about drugs—you’re reading about how the system works against you.
Pharmacy Reimbursement Models: How Laws Shape Generic Drug Payments
Discover how federal and state laws shape generic drug payments, why pharmacies struggle to stay open, and how the new Medicare $2 Drug List could change everything for patients and providers.
View More