When a patient walks in with shortness of breath, swollen ankles, or unexplained fatigue, the question isn’t just heart failure-it’s how fast can you rule it out? In emergency rooms and outpatient clinics across Australia and beyond, the answer increasingly starts with a single blood test: NT-proBNP. This isn’t just another lab order. It’s a game-changer for avoiding unnecessary scans, reducing hospital stays, and catching heart failure before it spirals.
What NT-proBNP Actually Measures
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein fragment released by the heart’s ventricles when they’re stretched from too much pressure or fluid. Think of it like a distress signal from the heart muscle. When the heart struggles-whether from high blood pressure, a weak pump, or valve problems-it releases this marker into the bloodstream. The test measures how much of that signal is present.
Unlike BNP, which breaks down quickly, NT-proBNP is stable in the blood for hours. That means labs can process it even if samples aren’t rushed. Roche’s Elecsys assay, the most common test used in Australia and the U.S., detects levels as low as 5 pg/mL. Results typically come back in under an hour in hospitals, and often within 90 minutes in clinics.
When You Should Order It-The Clear Indications
Don’t order NT-proBNP for every patient with a cough. But do order it when heart failure is even a remote possibility. Here’s when it’s essential:
- Acute dyspnea-especially in patients over 65. If someone comes in gasping for air, and you’re unsure if it’s heart failure, COPD, or a pulmonary embolism, NT-proBNP gives you the fastest objective answer.
- New-onset edema-swelling in the legs or abdomen without clear kidney or liver cause. A level above 1,200 pg/mL in someone over 75 raises red flags.
- Unexplained fatigue or reduced exercise tolerance-especially if they’ve been told they’re "just getting older." Heart failure can sneak in slowly.
- Post-acute coronary syndrome-even if the heart attack seems resolved, elevated NT-proBNP predicts higher risk of future events. The 2024 ACC/AHA guidelines now recommend it for risk stratification here.
- Monitoring known heart failure-levels that rise over weeks signal worsening, even if symptoms haven’t changed yet.
The European Society of Cardiology says this test is a Class I recommendation-meaning it’s not optional. It’s standard of care.
How to Interpret the Numbers-Age and Comorbidities Matter
There’s no single "normal" number. NT-proBNP naturally rises with age, kidney function, and other conditions. Ignoring this leads to false positives-and unnecessary stress, tests, and costs.
Here’s what the guidelines say:
- Under 50 years: Rule-out threshold is < 300 pg/mL. Anything above needs investigation.
- 50-75 years: Rule-out is < 900 pg/mL.
- Over 75 years: Rule-out is < 1,800 pg/mL.
But here’s where it gets tricky:
- Chronic kidney disease (CKD): Levels rise 28-40% in stage 3-4 CKD. Use a higher rule-out cutoff: < 1,200 pg/mL for patients with eGFR under 60.
- Obesity: Fat tissue suppresses NT-proBNP. A level of 400 pg/mL in a person with BMI 35 might mean the same as 700 pg/mL in someone lean.
- Atrial fibrillation: Even without heart failure, AFib can push levels up. Don’t panic-look at trends over time.
Dr. James Januzzi Jr. from Harvard puts it bluntly: "If NT-proBNP is below 300 pg/mL, you can confidently say it’s not acute heart failure. That’s 98% certainty."
Why NT-proBNP Over BNP?
Both tests measure heart stress. But NT-proBNP has clear advantages:
- Stability: NT-proBNP lasts longer in the blood-60 to 120 minutes. BNP degrades in 20. That means fewer false lows from delayed processing.
- Accuracy: A 2020 meta-analysis found NT-proBNP had a higher diagnostic accuracy (AUC 0.91) than BNP (0.88).
- Market dominance: In the U.S., 68% of natriuretic peptide tests are NT-proBNP. In Australia, adoption is now over 85% in major hospitals.
BNP still has a place-especially in rapid point-of-care settings. But for most labs and clinics, NT-proBNP is the default.
What NT-proBNP Can’t Do
It’s not a magic wand. Here’s where it fails:
- It doesn’t tell you the cause. A high level confirms heart stress, but not whether it’s from ischemia, hypertension, or valvular disease. You still need echo or MRI.
- It won’t help in asymptomatic screening. Medicare data shows 18% of tests are ordered in people with no symptoms. That’s overuse. Start with symptoms.
- It doesn’t replace clinical judgment. A 78-year-old with AFib, CKD, and an NT-proBNP of 850 pg/mL? That’s a gray zone. Combine it with history, exam, and maybe an ECG.
Dr. Allan Jaffe from Mayo Clinic warns: "NT-proBNP should never be used in isolation. It’s a tool-not a diagnosis."
Real-World Impact: Saving Time, Money, and Stress
One case from a Melbourne GP clinic: an 82-year-old woman with COPD came in with worsening breathlessness. Her NT-proBNP was 120 pg/mL. No heart failure. No echocardiogram. No admission. She got a steroid burst for her lungs instead. Saved $3,000. Avoided a day in the hospital. Reduced patient anxiety.
Across Australia, hospitals using NT-proBNP as a first-line test saw a 19% drop in unnecessary echocardiograms, according to the 2022 National Audit of Heart Failure. Emergency departments cut average stay times by 45 minutes.
And it’s not just cost. It’s peace of mind-for patients and clinicians.
What’s Changing in 2026?
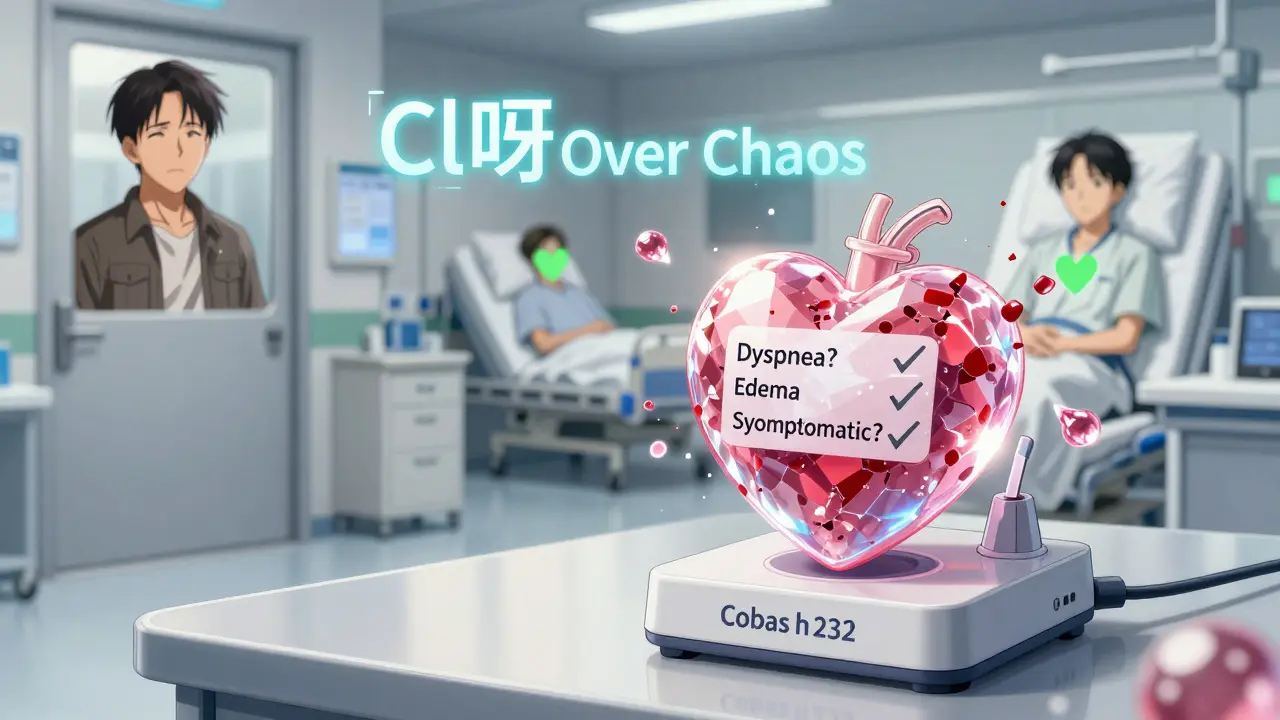
Point-of-care NT-proBNP devices are now rolling out in Australian GP clinics. The Roche Cobas h 232 delivers results in 12 minutes with 95% accuracy compared to lab tests. This means you can make decisions in the same visit.
Starting January 2025, Medicare began requiring prior authorization for NT-proBNP tests ordered without clear symptoms. This isn’t about limiting care-it’s about stopping waste. If you’re ordering it for a 50-year-old with no symptoms, no edema, no dyspnea? You’ll need to justify it.
The 2024 ACC/AHA/HFSA guidelines, expected in September, will expand NT-proBNP use to risk-stratify patients after heart attacks. If levels stay high after treatment, it means higher risk of death or rehospitalization. That’s a new tool for guiding long-term therapy.
Bottom Line: When to Order
Order NT-proBNP when heart failure is in the differential-and only when it changes management.
Don’t order it for:
- Asymptomatic patients
- Screening in healthy elderly without signs
- Patients with obvious non-cardiac causes (e.g., pneumonia, severe anemia)
Do order it for:
- Any patient with new or worsening dyspnea
- Unexplained fatigue or edema
- Post-heart attack with persistent symptoms
- Known heart failure with suspected deterioration
Remember: a level below 300 pg/mL rules out acute heart failure with near certainty. A level above 1,800 pg/mL in someone over 75? That’s a strong signal to act. But always pair it with clinical context. No number replaces listening to the patient.
NT-proBNP testing isn’t just a lab test. It’s a clinical decision-making shortcut. Use it right, and you’ll avoid unnecessary tests, reduce hospital admissions, and give patients faster answers. Use it wrong, and you’ll add noise to the signal.
Can NT-proBNP be used to diagnose heart failure in patients with kidney disease?
Yes, but you must adjust the interpretation. In patients with stage 3-5 chronic kidney disease (CKD), NT-proBNP levels are naturally higher due to reduced clearance. Use a higher rule-out threshold of <1,200 pg/mL instead of the standard <300 or <900 pg/mL. A level below 1,200 pg/mL still reliably excludes acute heart failure in CKD patients. However, elevated levels above this cutoff are less specific-you’ll need to combine it with echocardiography, clinical signs, and response to diuretics.
Is NT-proBNP testing covered by Medicare in Australia?
Yes, NT-proBNP testing is covered under Medicare Benefits Schedule (MBS) item 66002 for patients with suspected heart failure, acute dyspnea, or known heart failure requiring assessment. The rebate is approximately $45 AUD as of 2026. However, since January 2025, Medicare requires prior authorization if the test is ordered without clear clinical indications like dyspnea, edema, or reduced exercise tolerance. Ordering for asymptomatic screening or routine monitoring without justification may be denied.
How long does it take to get NT-proBNP results in a hospital vs. clinic?
In hospital laboratories, results are typically available within 45-60 minutes. In major Australian hospitals with on-site testing, turnaround can be as fast as 30 minutes. In outpatient clinics, samples are often sent to reference labs-results usually arrive within 24 hours. New point-of-care devices like the Roche Cobas h 232 can deliver results in under 12 minutes, and these are now being introduced in larger GP practices and emergency departments.
Can obesity affect NT-proBNP levels?
Yes. Fat tissue suppresses the release of natriuretic peptides. For every 5-unit increase in BMI, NT-proBNP levels drop by about 25-30%. This means a patient with severe obesity and heart failure might have a "normal" or only mildly elevated level, leading to underdiagnosis. Always interpret results in context. If clinical suspicion is high despite a low NT-proBNP, proceed with echocardiography rather than relying solely on the test.
Should NT-proBNP be repeated for monitoring heart failure?
Yes, but not routinely. NT-proBNP is most useful for monitoring when there’s a change in symptoms-like increased swelling, weight gain, or breathlessness. A rising level over weeks suggests worsening heart failure, even before symptoms are obvious. A falling level after starting treatment (like ACE inhibitors or SGLT2 inhibitors) indicates response. Don’t repeat it monthly without clinical reason. The 2023 Heart Failure Society guidelines recommend testing at diagnosis, after stabilization, and then only if symptoms change.
What’s the difference between NT-proBNP and BNP testing?
Both measure heart stress, but NT-proBNP is the inactive fragment, while BNP is the active hormone. NT-proBNP has a longer half-life (60-120 minutes vs. 20 minutes), making it more stable in blood samples. It’s also less affected by medication (like neprilysin inhibitors) and gives more consistent results across labs. BNP is slightly faster to process in point-of-care settings, but NT-proBNP is now the preferred test in 89% of Australian hospitals due to its reliability and accuracy.
Next Steps for Clinicians
If you’re not already using NT-proBNP routinely in suspected heart failure cases, start now. Keep the age-adjusted cutoffs handy. Learn the red flags: high levels in elderly patients with CKD or AFib need extra context. Talk to your lab about turnaround times and point-of-care options.
If you’re already using it, don’t stop there. Review your ordering patterns. Are you ordering it for asymptomatic patients? Are you adjusting for kidney disease? Are you combining it with clinical judgment? The test is powerful-but only when used wisely.




Angel Tiestos lopez
14 January, 2026 . 22:21 PM
bro this test is like the heart's SOS button 🚨 i remember my abuela went in with 'just tired' and they found fluid around her heart bc of this. no echo, no stress test, just a vial of blood and bam-answer. why do we still do 3-hour workups when we got this? 🤯
Pankaj Singh
15 January, 2026 . 16:12 PM
This is why American medicine is broken. You order a test because it's trendy, not because you listened to the patient. NT-proBNP is a crutch for lazy clinicians who don't want to do a physical exam. 18% of tests are ordered on asymptomatic people? That's not innovation-that's corporate lab greed.
Robin Williams
15 January, 2026 . 20:19 PM
YOOOO this is the future!!! Imagine walking into your GP, getting a finger prick, and in 12 mins you know if your heart’s crying or not?? No more waiting weeks for echo referrals. I’ve seen patients cry because they finally got an answer. This isn’t just a test-it’s hope in a vial. 🙌❤️ #HeartTechRevolution
Scottie Baker
16 January, 2026 . 09:27 AM
I swear to god if one more resident orders this on a 45-year-old with asthma and no edema I’m gonna lose it. We’re turning a diagnostic tool into a shotgun approach. You don’t need a blood test to know if someone’s wheezing from COPD. Stop overtesting. Stop overbilling. Stop pretending medicine is a checklist game.
Anny Kaettano
17 January, 2026 . 05:16 AM
The age-adjusted thresholds are critical-and often ignored. I had a 79-year-old with eGFR 42 and an NT-proBNP of 1,600. Clinically, she was fine. But if we used the <900 cutoff, we’d have flooded her with invasive tests. We need better education on comorbidities. This test is powerful, but it’s not a standalone oracle. Always pair it with clinical intuition.
Kimberly Mitchell
18 January, 2026 . 19:32 PM
Medicare requiring prior authorization? Long overdue. This test is being ordered like it’s a routine CBC. We’re drowning in noise. I’ve reviewed 37 charts this month where NT-proBNP was ordered for patients with pneumonia, anemia, or depression. It’s not diagnostic-it’s a waste of resources. Stop treating biomarkers like crystal balls.
Angel Molano
19 January, 2026 . 08:18 AM
If your NT-proBNP is above 1800 in someone over 75, you don’t need a PhD. You need to act. Stop overthinking. Start treating.
Vinaypriy Wane
21 January, 2026 . 04:25 AM
I appreciate the nuance here, especially regarding CKD and obesity... but I worry that the guidelines are still too rigid. I had a patient with BMI 40 and an NT-proBNP of 450-clinically, she was in early HF. If we followed the 'obesity suppresses levels' rule blindly, we’d have missed it. Context isn’t just age and kidney function-it’s also how the patient walks, breathes, and speaks. The numbers help, but they don’t replace presence.
Diana Campos Ortiz
21 January, 2026 . 18:21 PM
I’ve been using this test for 5 years now, and honestly? It’s changed how I talk to patients. Instead of saying 'we need to rule out heart failure,' I say 'let’s check your heart’s stress level.' It feels less scary. And when it’s under 300? I tell them, 'Your heart’s quiet-let’s look elsewhere.' That small shift reduces anxiety more than any scan ever could.
Jesse Ibarra
22 January, 2026 . 12:47 PM
Let’s be real-this isn’t about medicine. It’s about Roche’s bottom line. They pushed NT-proBNP because it’s more profitable than BNP. The 'higher accuracy' is statistically insignificant. The real reason? Labs make more money per NT-proBNP test. And now we’re all just dancing to their tune. Wake up. This isn’t science-it’s corporate marketing dressed in white coats.