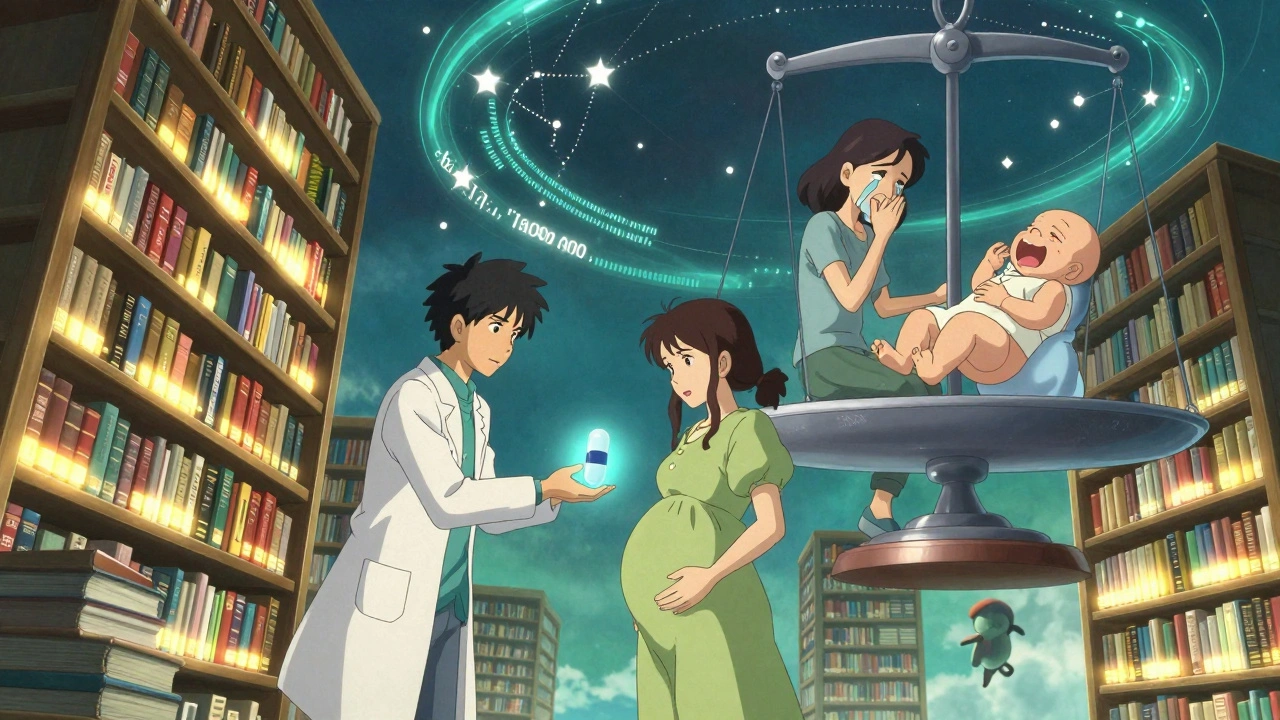
Pregnancy Antidepressant Safety Checker
Check Your Antidepressant Safety
Select your current medication to see evidence-based safety information for pregnancy
Depression During Pregnancy Is Common - And Dangerous If Left Untreated
One in seven pregnant people in the U.S. experiences depression. That’s not rare. It’s not unusual. It’s a medical reality. And when left untreated, it doesn’t just affect how you feel - it affects your baby’s health, too. Untreated depression increases the risk of preterm birth, low birth weight, and even preeclampsia. It also makes it harder to attend prenatal appointments, eat well, or get enough rest. The real danger isn’t the medication - it’s the silence around it.
SSRIs Are the First-Line Choice for a Reason
When medication is needed, doctors don’t reach for just any antidepressant. They pick SSRIs - selective serotonin reuptake inhibitors - because decades of research show they’re the safest option during pregnancy. Sertraline (Zoloft) and citalopram (Celexa) are the top choices. Why? Because they’ve been studied the most. More than 5 million pregnancies have been tracked in large, high-quality studies. The results? No clear link between these drugs and major birth defects, growth problems, or long-term developmental delays in children.
Fluoxetine (Prozac) is also used, but it carries a slightly higher risk of a rare condition called persistent pulmonary hypertension of the newborn (PPHN). That’s about 5 to 6 cases per 1,000 births, compared to 2 to 3 in babies not exposed to any antidepressants. Still, that risk is small. And when weighed against the dangers of untreated depression, it often tips the scale toward treatment.
Paroxetine Is the One SSRI to Avoid
Not all SSRIs are equal. Paroxetine (Paxil) stands out as the exception. Multiple studies show it carries a 1.5 to 2 times higher risk of heart defects in babies when taken during the first trimester. That’s why doctors don’t start new patients on paroxetine during pregnancy. And if you’re already taking it when you find out you’re pregnant? Your provider will likely help you switch to sertraline or citalopram as soon as possible. This isn’t fear-mongering - it’s evidence-based care.
Neonatal Adaptation Syndrome Is Temporary - Not Dangerous
Some babies exposed to SSRIs in the last trimester may have jitteriness, trouble feeding, or mild breathing issues after birth. This is called neonatal adaptation syndrome (PNAS). It happens in about 30% of exposed newborns. But here’s what matters: it’s not permanent. It doesn’t cause brain damage. It doesn’t lead to long-term problems. Symptoms usually fade within 2 weeks. Most babies need nothing more than extra cuddles, warm blankets, and close monitoring in the hospital. No long-term medication. No special care beyond what any newborn might need.
The Bigger Risk? Stopping Your Medication
Many women stop their antidepressants when they get pregnant - out of fear. But stopping cold turkey is risky. Studies show that 68% of women who quit their meds during pregnancy have a major depression relapse. That’s more than two out of three. Compare that to just 26% of women who stay on their medication. Relapse means more hospital visits, more emotional distress, and higher chances of self-harm. In fact, mental health conditions are the leading cause of pregnancy-related death in the U.S., accounting for nearly a quarter of all maternal deaths between 2017 and 2019.
One study found that antidepressant prescriptions for pregnant women dropped by 50% compared to the year before pregnancy. Yet, there was no increase in therapy or counseling to make up for it. That’s not safety - that’s a gap in care.
What About Birth Defects? The Data Says Otherwise
Early studies suggested SSRIs might slightly raise the risk of birth defects. But those studies didn’t account for one big thing: depression itself. Women with depression are more likely to smoke, drink, skip prenatal care, or have other health issues - all of which can affect a baby’s development.
When researchers compared women taking SSRIs to women with depression who didn’t take medication, the difference vanished. One major 2018 review found that when you control for mental illness, the risk of major birth defects with SSRIs drops to almost zero - an odds ratio of 1.04. That’s not a risk. That’s noise.
Long-Term Development? No Differences Found
Parents worry: will my child be different because of the meds? Will they have autism? ADHD? Learning problems?
A 2022 study tracked over 44,000 children in Norway from birth to age 5. Half were exposed to SSRIs in the womb. Half weren’t. The results? No difference in cognitive development, language skills, behavior, or autism rates. Other large studies in Sweden, Canada, and the U.S. agree. There’s no evidence that SSRIs cause long-term harm to a child’s brain.
What’s the Best Approach? One Drug. Lowest Dose. Close Monitoring.
Doctors don’t prescribe multiple antidepressants at once during pregnancy. That’s a recipe for complications. Instead, they recommend:
- Start with sertraline - it’s the most studied and safest.
- Use the lowest dose that controls your symptoms. No more. No less.
- Avoid switching meds in the first trimester unless absolutely necessary.
- Work with both your OB-GYN and a psychiatrist. This isn’t something to handle alone.
There’s no perfect pill. But sertraline comes closest. And if you’ve been stable on another SSRI before pregnancy? You probably shouldn’t change unless your provider says so. Stability matters more than theoretical risks.

Therapy and Lifestyle Matter Too
Medication isn’t the only tool. Cognitive behavioral therapy (CBT) is proven to help with depression during pregnancy. Regular walking, sunlight exposure, and good sleep hygiene can make a real difference. But these aren’t replacements for medication when your depression is moderate to severe. They’re partners - not substitutes.
If you’re struggling to find a therapist who understands perinatal mental health, ask your OB-GYN for a referral. Many hospitals now have integrated mental health teams for pregnant patients.
Don’t Panic Over the FDA Panel
In July 2025, a small FDA expert panel raised alarms about SSRIs during pregnancy. But their review was criticized by the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) as unbalanced and misleading. Only one of the ten panelists emphasized how critical these drugs are for preventing suicide and severe maternal decline.
ACOG called the panel’s findings “alarmingly unbalanced.” They warned that fear from such reports leads women to stop their meds - and that’s far more dangerous than any theoretical risk from the drugs.
What If You’re Already Pregnant and Taking Antidepressants?
Don’t stop. Don’t panic. Call your provider.
If you’re on paroxetine, switch to sertraline or citalopram. If you’re on fluoxetine and doing fine, you may not need to change. If you’re not on anything but feel overwhelmed, it’s not too late to start. Treatment can begin at any point in pregnancy - and it helps.
What you’re feeling right now - fear, guilt, confusion - is normal. But you’re not alone. Thousands of women take these medications safely every year. Their babies are healthy. Their lives are better.
Final Thought: Your Mental Health Is Part of Your Baby’s Health
There’s no such thing as a risk-free choice. But there is a riskier choice: silence. Untreated depression doesn’t just hurt you. It affects your baby’s development, your bond with them, and your ability to care for them after birth. SSRIs aren’t magic. But they’re one of the most studied, safest tools we have. And when used correctly, they help you become the parent you want to be - not the one depression tells you you’ll be.





John Biesecker
1 December, 2025 . 21:19 PM
i just found out i'm preggo and was on zoloft for 3 years 😅 i was terrified to tell my ob-gyn but she just nodded like 'yeah we do this all the time'... honestly? best decision i ever made. my baby's 6 months old and thriving. no autism, no jitteriness, just a happy little human who loves cuddles. 🤱❤️
Doug Hawk
3 December, 2025 . 19:33 PM
the data is clear but the fear is real. i get why people stop. i did too. first trimester. turned into a full-blown depressive episode by week 16. ended up in the hospital. never again. sertraline saved my life. and my daughter's. the real tragedy isn't the med-it's the silence. the stigma. the well-meaning but dangerous advice from auntie susan on facebook.
ruiqing Jane
3 December, 2025 . 19:42 PM
I've reviewed every longitudinal study on perinatal SSRI exposure across three continents. The effect sizes for neurodevelopmental outcomes are clinically insignificant. When confounders like maternal smoking, socioeconomic status, and untreated depression are properly controlled, the odds ratios converge near 1.0. This isn't speculation-it's meta-analytic consensus. Yet the misinformation persists because fear is more viral than data.
Michael Campbell
4 December, 2025 . 14:55 PM
they don't want you to know the truth. big pharma owns the FDA. they push these drugs so you'll stay dependent. your baby's brain is being rewired. you think it's safe? think again. my cousin's kid got autism after zoloft. they won't admit it but it's happening. #stopthelie
Saravanan Sathyanandha
5 December, 2025 . 16:36 PM
In India, we rarely discuss this. Depression in pregnancy? 'It's just hormones, beta.' But I’ve seen women break silently. One friend stopped her escitalopram because her mother-in-law said 'God will heal you.' She tried to end it all at 32 weeks. We got her to sertraline in time. The baby is fine. The mother? Still healing. But she’s alive. And that’s the only metric that matters.
Girish Padia
7 December, 2025 . 15:11 PM
this is why america is falling apart. you poison your own kids with chemicals just to feel 'better'. what happened to praying? to strong women? we used to endure. now we pop pills and call it progress. shame on you.
Carolyn Woodard
8 December, 2025 . 01:15 AM
The epidemiological signal for PPHN is statistically significant but clinically negligible when contextualized against the baseline risk of 2–3 per 1000. The absolute risk increase with fluoxetine is approximately 3 per 1000. When weighed against the 68% relapse rate upon discontinuation-and the documented increase in maternal suicidality, preterm delivery, and fetal growth restriction-the risk-benefit ratio overwhelmingly favors continuation. The real ethical failure lies in withholding evidence-based care under the guise of 'precaution'.
alaa ismail
9 December, 2025 . 16:06 PM
i was on prozac when i got pregnant. my doc said 'if you're stable, don't switch.' so i didn't. baby's 2 now. talks in full sentences, loves dinosaurs, sleeps through the night. no issues. the fear is louder than the science. but the science is still there.
Anthony Breakspear
10 December, 2025 . 10:51 AM
yo-just want to say this post is fire. i’m a dad. my wife was on sertraline during both pregnancies. we had two healthy kids, zero drama. people act like meds are some evil magic potion. nah. they’re like insulin for depression. you wouldn’t tell a diabetic to quit insulin because 'it's unnatural'. why are we so weird about mental health? 🙃
Zoe Bray
11 December, 2025 . 12:36 PM
It is imperative to underscore that the American College of Obstetricians and Gynecologists (ACOG), in conjunction with the Society for Maternal-Fetal Medicine (SMFM), has consistently affirmed the safety profile of sertraline and citalopram in gestational populations. The 2022 Norwegian cohort study, with its 44,000-child sample size and propensity score matching, provides the highest level of evidence to date. Disseminating misinformation undermines the foundation of perinatal psychiatry and endangers maternal autonomy.
Allan maniero
12 December, 2025 . 23:47 PM
I’ve been a midwife for 27 years. I’ve seen women cry because they think they’re monsters for taking antidepressants. I’ve seen babies born jittery, then smile at their moms two days later. I’ve seen women who stopped meds end up in the psych ward. And I’ve seen women who stayed on them hold their newborns like they’ve been waiting their whole lives to do it. The truth? Depression doesn’t care if you’re pregnant. It doesn’t pause. And neither should we. Let’s stop treating mental health like it’s optional. It’s not.
Fern Marder
13 December, 2025 . 12:35 PM
i'm not saying meds are bad... but maybe try yoga? or crystals? or just... being positive? 🌈✨ i mean, i got pregnant and just decided to vibe higher. no meds. baby's perfect. you just need to believe in yourself. 💖
Saket Modi
14 December, 2025 . 20:05 PM
why do people even bother reading this? it's just another big pharma ad. i'm out. 🤡
Genesis Rubi
16 December, 2025 . 07:00 AM
if you're american and on antidepressants while pregnant you're basically a traitor to the species. we used to be strong. now we're just chemical zombies. get a grip. your kid will pay for this. #americaisweak