Calcium channel blockers (CCBs) are one of the most commonly prescribed classes of heart medications. Millions of people take them daily for high blood pressure, chest pain, or irregular heartbeats. But here’s the thing most patients don’t know: calcium channel blockers don’t just work on your heart-they’re also deeply involved in how your body processes almost every other drug you take. The difference between safe use and dangerous side effects often comes down to one thing: metabolic interactions and drug clearance.
How Calcium Channel Blockers Work-and Why It Matters
Calcium channel blockers stop calcium from entering heart and blood vessel cells. This relaxes your arteries, lowers blood pressure, and slows down certain heart rhythms. But not all CCBs are the same. There are two main types: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine; and non-dihydropyridines (non-DHPs) like verapamil and diltiazem. DHPs mainly affect your blood vessels. That’s why amlodipine is the most prescribed CCB-it’s great for lowering blood pressure without messing much with your heart rate. Non-DHPs, on the other hand, hit both your heart and blood vessels. Verapamil and diltiazem can slow your heart rate, which is helpful for arrhythmias but risky if you’re already on other heart meds. The real issue isn’t just what these drugs do to your body-it’s how your body breaks them down.The Liver Is the Key Player
Almost all calcium channel blockers are processed by the liver, specifically by an enzyme called CYP3A4. This enzyme is responsible for breaking down more than half of all prescription drugs. When CCBs enter your body, CYP3A4 chops them up so they can be flushed out through your kidneys. But here’s the catch: many other drugs, foods, and even supplements use the same enzyme. If you take something else that also relies on CYP3A4, your liver gets overwhelmed. It can’t break down the CCB fast enough. That means more of the drug stays in your bloodstream. And when that happens, your blood pressure can drop too low, your heart can slow too much, or you can get dangerously dizzy. The numbers don’t lie. Amlodipine has about 64% oral bioavailability-meaning your body absorbs most of it. But verapamil? Only 20%. Why? Because the liver destroys most of it before it ever gets into your bloodstream. That’s why verapamil is more sensitive to interactions. If you block CYP3A4-even slightly-verapamil levels can spike by 60-70%.Biggest Culprits: Grapefruit, Antibiotics, and Antifungals
Grapefruit juice is the most talked-about offender. One glass can inhibit CYP3A4 for up to 72 hours. Studies show that people taking amlodipine with grapefruit juice have 40% higher drug levels in their blood. For verapamil? It’s worse-up to 70% higher. That’s why emergency rooms see so many cases of sudden, severe low blood pressure in older patients who started drinking grapefruit juice with their meds. Antibiotics like clarithromycin and antifungals like ketoconazole are even more dangerous. These drugs are strong CYP3A4 inhibitors. The FDA has issued multiple safety alerts about combining them with CCBs. In one study, patients on verapamil and clarithromycin had a 400% increase in verapamil levels. That’s not a typo. Four times the normal amount. Some ended up in the hospital with dangerously slow heart rates. Even over-the-counter meds can cause trouble. Some cold medicines contain pseudoephedrine or dextromethorphan, which can interfere with CYP3A4. And don’t forget St. John’s Wort. It does the opposite-it speeds up CYP3A4, making CCBs less effective. Patients on it often find their blood pressure creeping back up, even though they’re taking their pills regularly.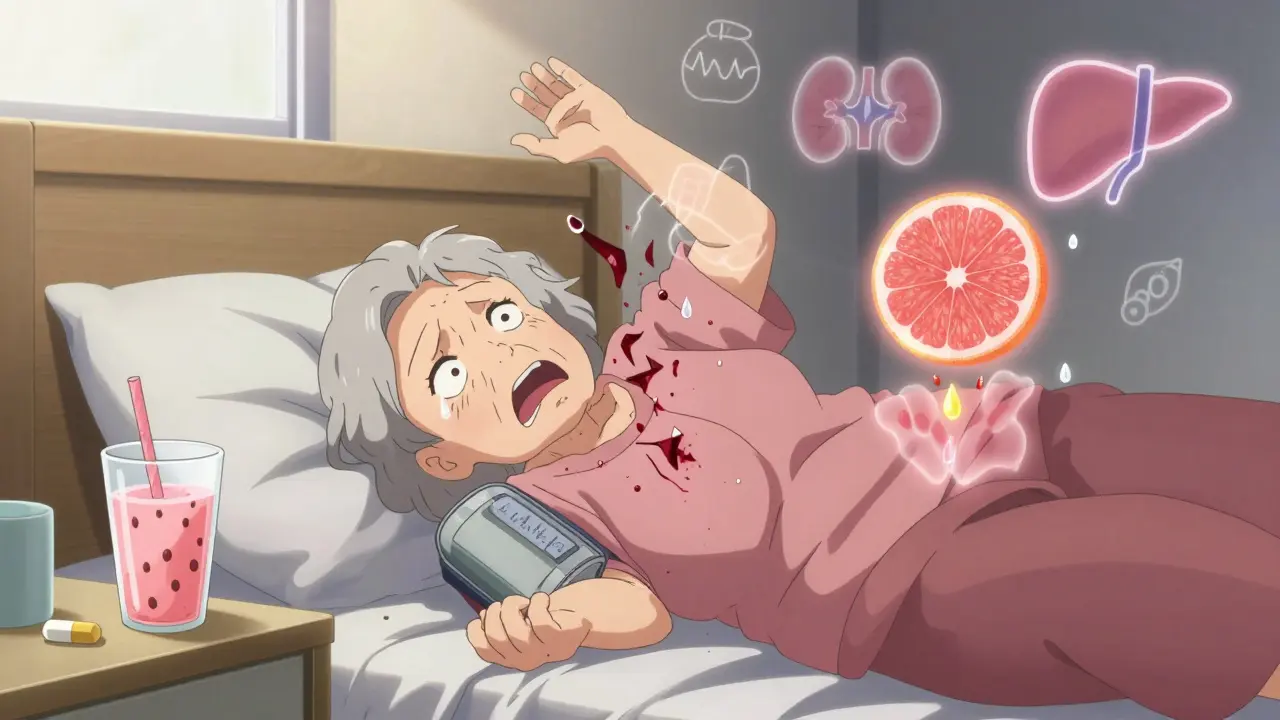
Why Amlodipine Is Often the Safest Choice
If you’re on five or more medications-common for people over 65-amlodipine is usually the best CCB option. Why? Because it barely inhibits CYP3A4. Unlike verapamil and diltiazem, it doesn’t interfere with how other drugs are broken down. It’s also long-lasting. One pill a day. No peaks and valleys in your blood levels. Studies show that only 12% of patients on amlodipine need dose adjustments when taking moderate CYP3A4 inhibitors. For diltiazem? That number jumps to 45%. Verapamil? Nearly half of patients need a change. That’s why doctors in Melbourne, Sydney, and across the U.S. are switching patients from verapamil to amlodipine when they start new meds. And here’s something surprising: amlodipine’s clearance isn’t affected much by kidney function. Even if your kidneys are a little weak, you usually don’t need to lower the dose. Verapamil? If your eGFR is below 60, you need to cut the dose by half. That’s a big deal for older adults.Real Stories, Real Risks
A 72-year-old woman in Adelaide was taking amlodipine for high blood pressure. She started using a grapefruit-flavored protein shake to help with her energy. Two weeks later, she passed out while walking her dog. Her blood pressure was 78/45. Her amlodipine level was 3 times higher than normal. She didn’t know grapefruit could do that. Another man in Brisbane was on verapamil for atrial fibrillation. His doctor added a low-dose statin for cholesterol. Within a week, he had muscle pain so bad he couldn’t climb stairs. Turns out, verapamil and statins both use CYP3A4. Together, they caused rhabdomyolysis-a rare but life-threatening muscle breakdown. He needed hospitalization. These aren’t rare cases. On patient forums, 73% of negative reviews about CCBs mention side effects linked to interactions. The most common complaint? Unexpected dizziness or fainting. The second? Muscle pain or weakness. Both are signs your body can’t clear the drugs properly.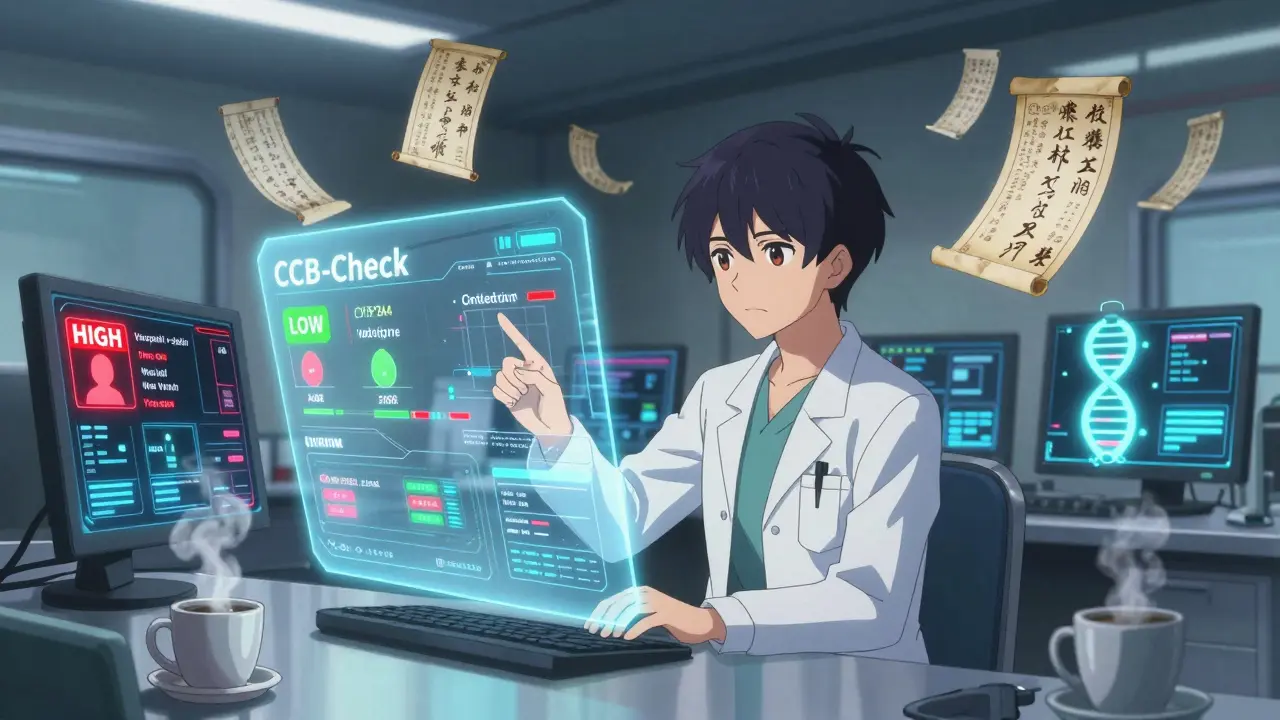
What You Should Do
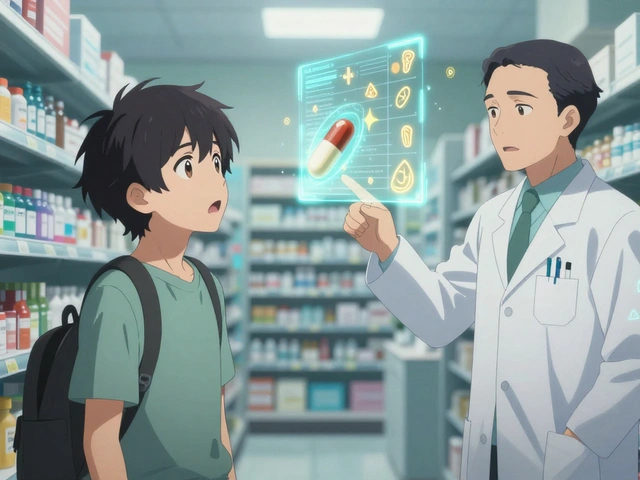
If you take a calcium channel blocker, here’s what you need to do:- Make a list of every medication, supplement, and herbal product you take-including what you get over the counter.
- Ask your pharmacist: “Could any of these affect my blood pressure or heart rate?”
- Avoid grapefruit, Seville oranges, and pomelos completely if you’re on verapamil or diltiazem.
- If you’re over 65 or have kidney problems, ask if amlodipine might be safer than your current CCB.
- Watch for signs of too much drug: dizziness, swelling in your ankles, slow heartbeat, or extreme fatigue.
What Doctors Are Doing Now
Hospitals and clinics are catching on. Electronic health records now flag potential CCB interactions automatically. If you’re prescribed a CCB and an antibiotic like clarithromycin, your doctor’s system will pop up a warning. Some systems even suggest alternatives. In 2023, the FDA approved a new tool called CCB-Check. It scans your meds and gives a risk score-low, medium, or high-for interactions. Hospitals using it saw a 31% drop in hospitalizations from CCB-related problems in just six months. Genetic testing is also becoming more common. About 27% of people have a gene variant that makes CYP3A4 work slower. These people need lower CCB doses from the start. It’s not routine yet-but it’s coming.The Bottom Line
Calcium channel blockers save lives. But they’re not harmless. Their real danger isn’t the drug itself-it’s what happens when they meet other drugs, foods, or even your own genetics. The liver doesn’t distinguish between your blood pressure pill and your grapefruit smoothie. It just tries to process them all at once. If you’re on a CCB, don’t assume it’s safe just because your doctor prescribed it. Talk to your pharmacist. Ask about interactions. Get your meds reviewed every six months. And if you feel unusually tired, dizzy, or weak-don’t wait. That could be your body telling you your drug levels are too high. The future of CCB use isn’t about finding a better drug. It’s about understanding how your body handles them-and making smarter choices with every pill you take.Can I drink grapefruit juice while taking a calcium channel blocker?
No, it’s not safe if you’re taking verapamil or diltiazem. Grapefruit juice blocks the CYP3A4 enzyme, causing these drugs to build up in your blood. This can lead to dangerously low blood pressure, slow heart rate, or even heart failure. Even amlodipine, which is safer, can have its levels increased by 40% with grapefruit. The safest choice is to avoid grapefruit, Seville oranges, and pomelos entirely while on any calcium channel blocker.
Which calcium channel blocker has the fewest drug interactions?
Amlodipine has the fewest interactions among calcium channel blockers. Unlike verapamil and diltiazem, it doesn’t significantly inhibit CYP3A4 or P-glycoprotein. It’s also metabolized slowly and steadily, making it less sensitive to changes in liver function. For patients on multiple medications-especially older adults-amlodipine is the preferred choice because it’s less likely to cause dangerous interactions with antibiotics, statins, or antifungals.
Why does my doctor check my kidney function before prescribing a calcium channel blocker?
While most calcium channel blockers are cleared by the liver, their metabolites are removed by the kidneys. If your kidneys aren’t working well (eGFR below 60), those metabolites can build up. Verapamil and diltiazem require dose reductions in patients with reduced kidney function. Amlodipine, however, doesn’t need adjustment-even with moderate kidney impairment-because less than 1% of the drug is excreted unchanged. That’s why kidney tests help doctors pick the safest option.
Can calcium channel blockers cause muscle pain?
Yes, especially when taken with statins like simvastatin or atorvastatin. Verapamil and diltiazem slow down how fast your liver breaks down statins, causing them to build up. This can lead to muscle pain, weakness, or a rare but serious condition called rhabdomyolysis. Amlodipine doesn’t have this effect, so it’s often switched to when patients on statins develop muscle symptoms. If you’re on a CCB and a statin and feel new muscle soreness, tell your doctor immediately.
Are there genetic factors that affect how calcium channel blockers work?
Yes. About 27% of people have genetic variants in the CYP3A4 enzyme that make it work slower. These people break down CCBs like verapamil and diltiazem much more slowly, so they’re at higher risk of side effects even at normal doses. Testing for these variants isn’t routine yet, but research is advancing quickly. In the next few years, personalized dosing based on genetics may become standard practice, especially for older patients on multiple drugs.





Samyak Shertok
16 January, 2026 . 16:35 PM
So let me get this straight - we’re all just lab rats in a pharmaceutical soap opera? One glass of grapefruit juice and suddenly your heart’s on vacation? I mean, if the liver’s a bouncer, why’s it letting in every drug but kicking out the ones we actually need? 🤔
Stephen Tulloch
17 January, 2026 . 22:53 PM
Amlodipine is the only CCB that doesn’t act like a drama queen. Verapamil? More like vera-panic. If you’re on 5 meds and still using grapefruit juice, you’re not managing your health - you’re performing a one-man TED Talk on how to die young. 🍊💀
vivek kumar
18 January, 2026 . 16:31 PM
The enzymatic competition at CYP3A4 is not merely a pharmacological footnote - it is a systemic vulnerability in modern polypharmacy. The fact that 73% of negative CCB reviews cite interaction-induced side effects suggests a systemic failure in patient education, not a drug flaw. We must reframe this as a public health literacy crisis.
Henry Ip
19 January, 2026 . 16:39 PM
This is actually super useful. I’ve been on amlodipine for years and never knew grapefruit could mess with it. Just asked my pharmacist to check all my supplements - turns out my turmeric gummies might be a problem too. Good reminder to always ask
Isabella Reid
20 January, 2026 . 05:26 AM
I love how this post doesn’t just say ‘don’t drink grapefruit juice’ - it explains why. My grandma took verapamil and drank grapefruit smoothies every morning. She didn’t know it was dangerous. This needs to be shared with older folks who trust their juice more than their doctors.
kanchan tiwari
21 January, 2026 . 10:24 AM
This is all a lie. Big Pharma doesn’t want you to know that CYP3A4 is a distraction. The real issue? The FDA’s been paid off by the citrus industry. Grapefruit is a natural detox. They’re scared because people might stop taking pills if they knew they could just eat fruit. #CancerCureExposed
Bobbi-Marie Nova
22 January, 2026 . 03:36 AM
So basically if you’re over 65 and on meds, your life is one smoothie away from an ER visit? 🙃 I’m just glad I stick to orange juice. And maybe a little wine. And my 3 daily vitamins. And that herbal tea. Wait…
Allen Davidson
23 January, 2026 . 22:19 PM
Great breakdown. I’ve seen so many patients on verapamil get thrown into a tailspin when their doc adds a new antibiotic. Switching to amlodipine is often the safest move - especially for seniors. Don’t wait for a crash to ask about alternatives.
john Mccoskey
25 January, 2026 . 05:18 AM
The entire paradigm of pharmacokinetic interaction is a symptom of a deeper pathology: the commodification of human biology. We reduce complex metabolic pathways to algorithmic risk scores, then call it ‘precision medicine.’ Meanwhile, patients are left to navigate a labyrinth of warnings written in legalese while being told to ‘just take your pills.’ The system isn’t broken - it’s designed to fail you slowly.
Joie Cregin
25 January, 2026 . 16:20 PM
I’ve got a cousin who’s 70 and takes five meds. She swears by her grapefruit every morning. I’m sending her this article. She’ll roll her eyes, but she’ll read it. And maybe - just maybe - she’ll swap it for a banana. She’s stubborn but not stupid.
Rob Deneke
26 January, 2026 . 22:42 PM
Amlodipine is the way to go if you’re on other meds. I switched from diltiazem after my statin gave me muscle pain. No more issues. Simple. One pill a day. No drama
Chelsea Harton
28 January, 2026 . 04:01 AM
Grapefruit juice bad for ccb. Amlodipine good. Just dont mix stuff. Thx for the info
Corey Chrisinger
29 January, 2026 . 05:34 AM
It’s wild how our bodies are these tiny biochemical factories, and we just toss in pills like they’re ingredients in a soup. But the liver? It’s the chef who’s been working 80-hour weeks and now has to cook 17 dishes at once. No wonder it burns the food.
Bianca Leonhardt
30 January, 2026 . 21:37 PM
If you’re still taking verapamil after reading this, you’re either a medical professional who knows better… or you’re just gambling with your life. No excuses.
Travis Craw
1 February, 2026 . 07:16 AM
I used to drink grapefruit juice with my meds. Didn’t think it mattered. Now I just stick to water. My BP’s been stable since. Thanks for the wake-up call. I’ll pass this to my mom too.