When you pick up a prescription, you might see a generic version on the shelf instead of the brand-name drug you asked for. You might wonder: Is it really the same? Does it work just as well? Is it safe? These aren’t just questions patients ask - they’re questions that have been studied for decades. And the answer, most of the time, is yes. But not always. And that’s where things get real.
What Makes a Generic Drug ‘Equal’?
Generic drugs aren’t copies. They’re scientifically proven duplicates. The U.S. Food and Drug Administration (FDA) requires them to contain the exact same active ingredient, in the same strength, and delivered the same way - whether it’s a pill, injection, or inhaler. That’s the easy part. The hard part? Proving your body absorbs it the same way.
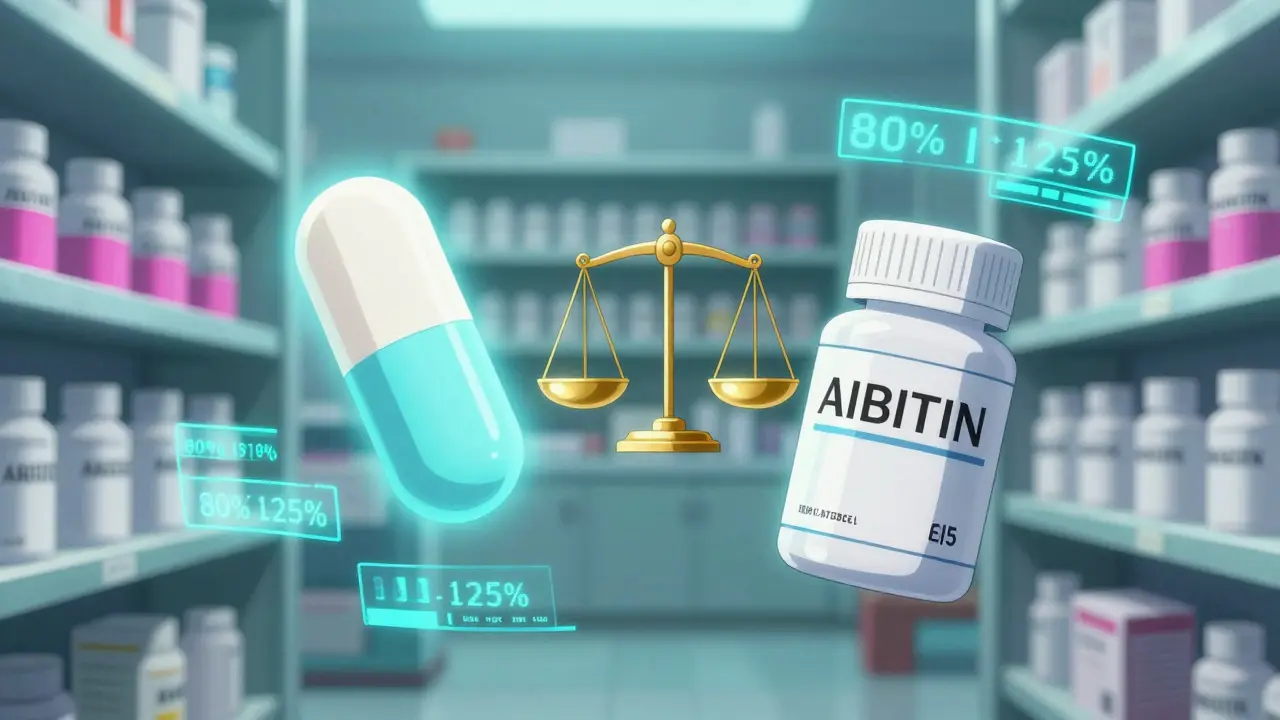
To get approved, a generic drug must pass a bioequivalence study. These aren’t theoretical. They’re done with real people - usually 24 to 36 healthy volunteers. Researchers measure how much of the drug enters the bloodstream and how fast. The gold standard? The 90% confidence interval for the ratio of the generic to brand-name drug must fall between 80% and 125% for both peak concentration (Cmax) and total exposure (AUC). That’s not a guess. That’s a hard scientific bar.
Between 1996 and 2007, the FDA reviewed over 2,000 of these studies. Not one showed a meaningful difference in how the body handled the drug. That’s not luck. That’s rigor.
Real-World Results: Do Generics Actually Work?
Lab results don’t always tell the whole story. What happens when millions of people take generics every day for years?
A massive 2020 study tracked nearly all insured people in Austria between 2007 and 2012. Researchers compared outcomes for 17 common chronic disease drugs - things like blood pressure meds, diabetes pills, and cholesterol reducers. The results? Generics were linked to fewer deaths in 10 of the 17 drugs. Fewer heart attacks and strokes in 11. After adjusting for age, income, and other factors, the five-year survival rate for people on generics was 82.7%, compared to 79.8% for those on brand-name versions. That’s not a tiny difference. That’s life-saving.
Another study looked at 3.5 million patients in the U.S. using generics for high blood pressure, diabetes, osteoporosis, and depression. The results? No difference in hospital visits, heart events, or symptom control. In fact, for amlodipine (a blood pressure drug), people on the generic version had a 9% lower risk of heart problems than those on the brand.
Medicare data from 2021 shows 68% of seniors on generic heart medications said they felt no difference in how well they worked. Only 22% reported minor side effects - and most of those went away over time.
When Generics Don’t Work - The Exceptions
There’s a reason your doctor sometimes writes ‘dispense as written’ on a prescription. It’s not because they don’t trust generics. It’s because some drugs are unforgiving.
Drugs with a narrow therapeutic index - where even a tiny change in blood level can cause harm - need extra caution. Think thyroid meds like levothyroxine, seizure drugs like phenytoin or lamotrigine, and blood thinners like warfarin.
A 2023 study in Epilepsia found that switching between different generic versions of levetiracetam led to an 18% higher chance of seizures. Not because the drug was bad. But because different manufacturers use slightly different inactive ingredients. For some people, those differences affect how the pill dissolves in the stomach. That’s enough to throw off seizure control.
Patients on Reddit and pharmacy forums regularly report switching between generic brands of levothyroxine and suddenly feeling exhausted, gaining weight, or having trouble concentrating. One person wrote: ‘I tried three generics for Synthroid. Only one kept my TSH stable.’ That’s not anecdotal. That’s a pattern.
A 2013 study documented a patient whose symptoms from a bacterial infection didn’t improve on generic levofloxacin - until they switched back to the brand-name version. Within 10 days, they were fine. That’s rare. But it happens.

Why Do Some People Think Generics Don’t Work?
It’s not always the drug. Sometimes it’s the mind.
Studies show that if you believe a generic is inferior, you’re more likely to notice side effects or feel like it’s not working. This is called the ‘generic perception bias.’ It’s real. And it’s powerful.
One 2019 study found that patients who knew they were taking a generic were more likely to report side effects - even when the actual drug was identical to the brand. Their expectations shaped their experience.
Pharmacists report that 42% of patients express concern about generic quality before even trying it. That’s not because generics are unsafe. It’s because the message they’ve heard - from ads, from friends, from TV - is that ‘brand means better.’
But here’s the flip side: 78% of GoodRx users who reviewed generic medications gave them 4 or 5 stars, saying they worked just as well - at a fraction of the cost.
What Do Doctors and Pharmacists Really Think?
Most doctors trust generics. A 2020 survey found that 87% of physicians have confidence in generic drugs. But specialists - neurologists, endocrinologists, cardiologists - are more cautious. They’ve seen the exceptions.
The FDA’s Orange Book is the official guide to therapeutic equivalence. It rates generics as ‘A’ (therapeutically equivalent) or ‘B’ (possible differences). If your drug is rated ‘A,’ you can switch with confidence. If it’s ‘B,’ your doctor should know.
Pharmacists are trained to substitute generics unless told otherwise. In 2022, only 3.2% of prescriptions had a ‘dispense as written’ note. That means 97% of the time, the system is working as intended.
But here’s what many don’t tell you: if you switch from one generic to another - say, from Teva to Mylan - you’re still switching. And for some drugs, that matters.
Cost vs. Risk: The Bottom Line
Generics save the U.S. healthcare system over $377 billion every year. Since 2006, Medicare has saved $1.67 trillion thanks to generics. That’s not just money. That’s access. It’s people who can afford their meds. It’s fewer skipped doses. It’s fewer ER visits.
For 90% of prescriptions, the science is clear: generics are just as safe and effective. They’re not cheaper because they’re worse. They’re cheaper because they don’t need to pay for marketing, TV ads, or patent lawsuits.
But for the 5-10% of drugs with narrow therapeutic windows - thyroid, epilepsy, blood thinners - consistency matters. Stick with the same generic manufacturer if it works for you. Don’t switch unless your doctor says so. And if you notice a change in how you feel after a switch, tell your provider. Don’t assume it’s ‘all in your head.’
The system works. But it’s not perfect. And that’s okay. The goal isn’t perfection. It’s safety, effectiveness, and access - all at the same time. Generics deliver that. Most of the time. And when they don’t, we know why. And we know what to do.
What Should You Do?
- If you’re on a routine medication - blood pressure, cholesterol, diabetes, depression - stick with the generic. It’s safe, proven, and saves you hundreds a year.
- If you’re on a narrow therapeutic index drug - thyroid, seizure meds, blood thinners - ask your pharmacist: ‘Which generic manufacturer do I have?’ Write it down. Don’t switch unless you have to. And if you do, monitor how you feel.
- If you feel different after a switch - tired, anxious, dizzy, seizures returning - don’t ignore it. Call your doctor. Bring your pill bottle. It’s not ‘all in your head.’ It might be the filler.
- If you’re worried about quality - remember: the FDA inspects every generic factory. The same ones that make brand-name drugs often make the generics. The only difference? The label.
Are generic drugs as effective as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generics to prove they work the same way in the body as the brand-name version through strict bioequivalence testing. Large studies involving millions of patients show no meaningful difference in outcomes for conditions like high blood pressure, diabetes, and depression. Generics are not ‘weaker’ - they’re identical in active ingredients and performance.
Why do some people say generics don’t work for them?
For most people, it’s not the drug - it’s perception or switching between different generic manufacturers. Some medications, like levothyroxine or lamotrigine, are sensitive to small changes in inactive ingredients. Switching between brands of the same generic can sometimes cause symptoms to return. Also, if you believe a generic is inferior, you may notice side effects more - a psychological effect called ‘generic perception bias.’
Which drugs should I avoid switching to generics?
Avoid switching generics for drugs with a narrow therapeutic index - where small changes in blood levels can cause serious effects. These include levothyroxine (thyroid), warfarin (blood thinner), phenytoin and lamotrigine (seizure meds), and some psychiatric drugs like lithium. Always check with your doctor before switching. The FDA’s Orange Book lists which generics are rated ‘A’ (safe to substitute) or ‘B’ (potential differences).
Can I trust generics made overseas?
Yes. The FDA inspects all manufacturing facilities - whether in the U.S., India, China, or elsewhere - before approving a generic drug. Over 80% of generic drugs sold in the U.S. are made overseas, but they must meet the same standards as U.S.-made drugs. The 2021 valsartan recall was due to contamination - not because it was foreign-made, but because a single supplier failed quality control. That’s rare, and it’s caught.
Why are generics so much cheaper?
Generics don’t pay for advertising, brand marketing, or patent protection. Once a brand-name drug’s patent expires, other companies can make the same molecule. They don’t need to repeat expensive clinical trials - just prove bioequivalence. That cuts costs by 80-85%. The savings go to you, your insurer, and the healthcare system - not to shareholders.
Should I ask my doctor to prescribe the brand name?
Only if you’ve had a bad reaction to a generic, or if you’re on a narrow therapeutic index drug and the generic isn’t working. Otherwise, there’s no medical reason to pay more. If your doctor says ‘dispense as written,’ it’s usually because they’re being cautious - not because generics are unsafe. Ask why. Most of the time, the answer will be: ‘It’s fine.’





Glendon Cone
1 January, 2026 . 09:51 AM
Been taking generic lisinopril for 5 years now. No issues. Saved me $120/month. My BP is better than when I was on the brand. 🤙
Colin L
1 January, 2026 . 12:52 PM
Look, I get it, the FDA says it’s all good, but have you ever actually talked to someone who switched from Synthroid to a generic and then spent six months feeling like a zombie, gaining 20 pounds, and crying uncontrollably in the cereal aisle? No? Well, I have. And it’s not ‘perception bias’-it’s pharmacology. The inactive ingredients? They’re not inert. They’re like the seasoning in a soup-change the salt, change the whole damn flavor. And when you’re talking about a hormone that regulates your entire metabolism, you don’t want some factory in Mumbai deciding your thyroid gets a different binder than your neighbor’s. The system works? Maybe. But it’s not flawless. And pretending it is is what got us into this mess in the first place.
Hayley Ash
2 January, 2026 . 19:17 PM
Wow. So the FDA is basically a glorified stamping machine and your doctor is just a glorified cashier? 😂
henry mateo
4 January, 2026 . 08:51 AM
i had the same thing happen with my levothyroxine. switched from teva to mylan and suddenly i was exhausted all the time. went back to teva and boom, energy back. i didnt think it was real til i read this post. thanks for putting it out there. its not just me.
Kunal Karakoti
5 January, 2026 . 03:45 AM
It's interesting how we equate cost with quality. If a drug is cheaper, we assume it's lesser. But isn't that a reflection of our cultural conditioning? The brand name carries the illusion of superiority, while the generic carries the truth of efficiency. Perhaps the real question isn't whether generics work-but why we're so afraid of them.
Kelly Gerrard
6 January, 2026 . 20:19 PM
Stop coddling patients. If your thyroid meds aren't working, see your doctor. Don't blame the generic. You're not special. The science is clear. Get over it.
Henry Ward
6 January, 2026 . 22:08 PM
Of course the FDA says generics are fine. They’re paid by the same pharma lobby that profits off brand names. Wake up. The system is rigged. You think they want you to save money? They want you addicted to overpriced pills. This is corporate propaganda dressed as science.
Aayush Khandelwal
8 January, 2026 . 08:54 AM
Let’s not conflate bioequivalence with bioidentity. The active moiety may be identical, but the pharmacokinetic orchestra-absorption, dissolution, transit time-is modulated by excipients. In narrow TI drugs, even a 5% variance in Tmax can trigger a cascade. It’s not superstition-it’s pharmacodynamics. The FDA’s ‘A’ rating is a heuristic, not a guarantee. Context is king.
Sandeep Mishra
9 January, 2026 . 17:29 PM
Hey everyone, I’ve been a pharmacist for 18 years. I’ve filled thousands of generics. Most patients never notice a difference. But if someone says they feel different after a switch? I listen. No judgment. I check the manufacturer. I check their TSH. I check their mood. Because sometimes, it’s the filler. Sometimes, it’s the mind. And sometimes, it’s both. Be kind. Be patient. And if you’re unsure? Ask your pharmacist. We’re here to help, not to judge.
Joseph Corry
9 January, 2026 . 17:40 PM
How quaint. You believe in regulatory oversight and population-level data? How... bourgeois. The real truth is that medicine is a narrative. The generic is the proletariat’s version of the brand’s myth. You don’t need science-you need a story. And the story you’re being sold is that equality is achievable through cost reduction. How poetic. How tragic.
kelly tracy
11 January, 2026 . 07:57 AM
Oh please. I switched to generic lamotrigine and had a seizure. Then I switched back. Boom. Fine. So now I’m supposed to just accept that my life is a statistical outlier? I’m not a data point. I’m a person. And you’re all just here to pat yourselves on the back for being ‘rational.’
srishti Jain
12 January, 2026 . 04:44 AM
generic = bad. period. my cousin died from it. dont argue.
Cheyenne Sims
13 January, 2026 . 21:51 PM
As an American taxpayer, I find it offensive that foreign manufacturers are allowed to produce life-saving medications under the same standards as U.S. facilities. This is not national security. This is national surrender.