Colchicine-Macrolide Interaction Checker
Check Your Medication Combination
This tool helps you determine if your current or prescribed antibiotic is safe to take with colchicine.
Key Safety Facts
- Clarithromycin can quadruple colchicine levels
- 2.3x higher risk of toxicity with clarithromycin/erythromycin
- Switching to azithromycin reduces risk by 92%
- Risk increases with kidney disease and age
Result
Please select an antibiotic and click "Check Interaction Risk" to see your result.
Imagine taking a simple pill for gout or heart inflammation, then getting a prescription for an antibiotic like clarithromycin for a chest infection. Sounds harmless, right? But this common combo can send your body into a tailspin-leading to muscle breakdown, organ failure, or even death. The problem isn’t the drugs themselves. It’s what happens when they meet inside your body.
Why This Interaction Is So Dangerous
Colchicine has been used for centuries to treat gout. Today, it’s also prescribed after heart attacks and for recurring pericarditis. But its safety margin is razor-thin. The difference between a therapeutic dose and a toxic one is tiny. Normally, your body keeps colchicine levels in check using two main systems: CYP3A4 enzymes in your liver and gut, and P-glycoprotein (P-gp) transporters that pump the drug out of cells. When you add a macrolide antibiotic like clarithromycin or erythromycin, both of these safety systems get shut down. CYP3A4 slows down, so colchicine doesn’t break down. P-gp stops working, so colchicine piles up inside your cells. Together, this can quadruple colchicine levels in your blood. At concentrations above 3.3 ng/mL, especially in people with kidney issues, toxicity kicks in.Not All Macrolides Are the Same
You might think all antibiotics in the macrolide family are equally risky. They’re not. Clarithromycin is the worst offender. It’s a strong inhibitor of both CYP3A4 and P-gp. Studies show it can raise colchicine levels by up to 400%. Erythromycin is less potent but still dangerous. Azithromycin? Almost no interaction. It barely touches CYP3A4 or P-gp. This isn’t just theoretical. A 2022 study of over 12,000 patients found those taking colchicine with clarithromycin or erythromycin had a 2.3 times higher risk of serious toxicity-like low white blood cell counts, muscle damage, or kidney failure. But those on azithromycin? No increased risk. That’s a critical distinction. Switching from clarithromycin to azithromycin cuts the danger by 92%.What Happens When Toxicity Strikes
Colchicine toxicity doesn’t come with a warning label you can easily spot. Early signs-nausea, vomiting, diarrhea-are often mistaken for a stomach bug. By the time muscle pain, weakness, or unexplained bruising show up, it’s often too late. The FDA’s adverse event database from 2015 to 2020 recorded 147 cases of colchicine toxicity linked to macrolides. Sixty-three percent involved clarithromycin. A 2019 case series described 12 patients who developed rhabdomyolysis, multi-organ failure, or severe neutropenia after taking standard colchicine doses with clarithromycin. Three died. Emergency doctors report seeing this more often than rheumatologists. Why? Because when a patient comes in with chest pain and gets prescribed colchicine, then later develops pneumonia and gets antibiotics, the connection isn’t always made. Many patients don’t mention they’re taking colchicine for heart inflammation, assuming it’s just an “old gout pill.”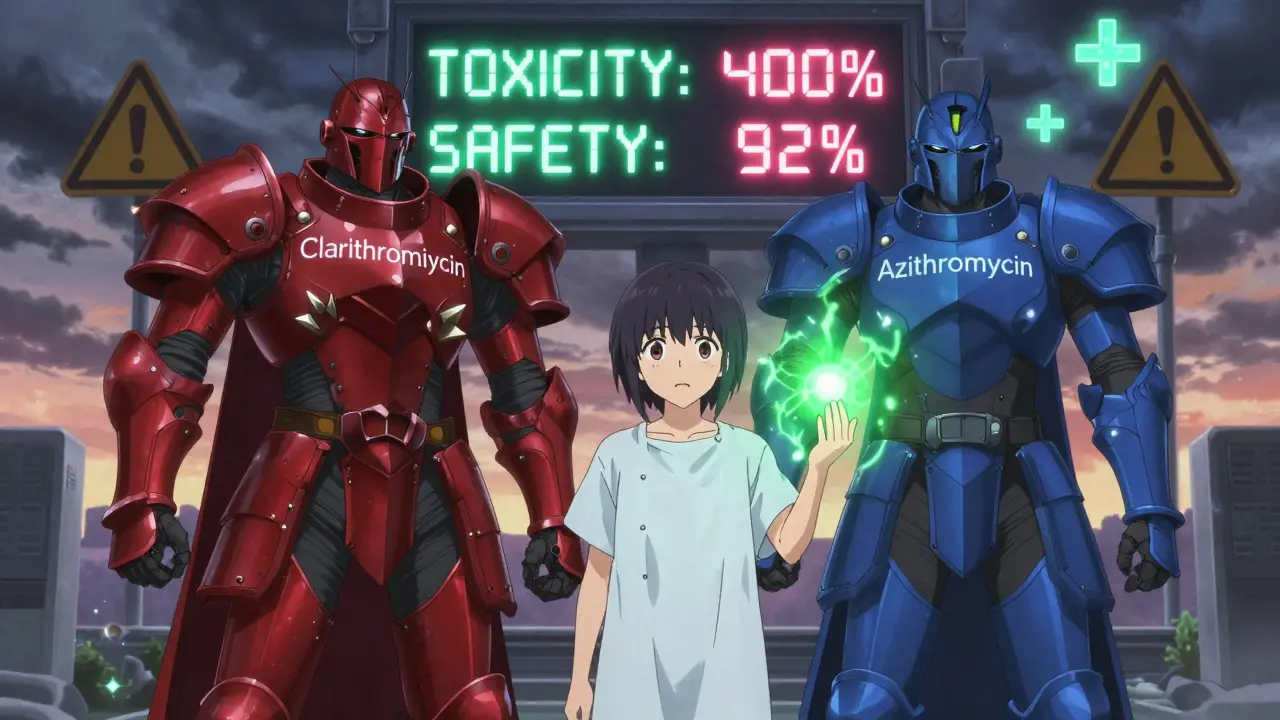
Who’s at Highest Risk?
Not everyone who takes this combo will get sick. But certain people are sitting on a ticking clock:- People over 70
- Those with kidney disease (even mild)
- Patients on multiple medications
- Anyone taking other CYP3A4 or P-gp inhibitors-like diltiazem, verapamil, amiodarone, or even some antifungals
What Doctors Are Doing About It
Guidelines from the American College of Rheumatology and the American College of Cardiology are clear: Don’t combine colchicine with clarithromycin or erythromycin. If you must use a macrolide, pick azithromycin. If no alternative exists, cut the colchicine dose in half and monitor closely. But here’s the problem: most electronic health records still don’t flag this interaction well. A 2023 survey of 245 physicians found that 68% had seen at least one case of this interaction in practice. Only 37% of U.S. hospitals can test colchicine blood levels routinely. Without that, doctors are flying blind. A 2024 study showed that when Epic’s EHR system added a tiered alert system-red alerts for clarithromycin, yellow for erythromycin-prescribing errors dropped by 63%. That’s not magic. It’s smart design.
What You Can Do Right Now
If you’re taking colchicine:- Ask your doctor or pharmacist: Is this antibiotic safe with colchicine?
- Never take clarithromycin or erythromycin if you’re on colchicine-unless you’ve discussed alternatives.
- Switch to azithromycin if possible. It works just as well for most infections.
- If you’re on a long-term colchicine regimen (like after a heart attack), keep a list of all your meds-including supplements. Some herbal products, like St. John’s wort or grapefruit juice, also interfere with CYP3A4.
- Watch for early warning signs: unexplained muscle pain, extreme fatigue, dark urine, fever, or unusual bruising. Call your doctor immediately.
The Bigger Picture: Why This Matters
Colchicine use has exploded since 2010. It’s cheap-under $50 a year-and effective. Alternatives like canakinumab cost nearly $200,000. So hospitals and insurers keep pushing it. But that means more people are on it. And more people are getting antibiotics. We’re talking about an estimated 1.2 million Americans every year who could be exposed to this dangerous combo. That’s not a rare event. It’s a systemic blind spot. New research is trying to fix this. Takeda is testing a new version of colchicine-COL-098-that doesn’t interact with P-gp. Early trials show it’s 92% safer with clarithromycin. Genetic testing is also becoming more accessible. A 2023 study found that two common gene variants (CYP3A5*3/*3 and ABCB1 3435C>T) predicted 78% of toxicity cases. Soon, we may be able to personalize colchicine dosing based on your DNA. But until then, the best tool you have is awareness. This isn’t a complex pharmacology puzzle. It’s a simple rule: Never mix colchicine with clarithromycin or erythromycin. Azithromycin is your safe bet. And if you’re unsure-ask.Can I take azithromycin with colchicine?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-gp, so it’s considered safe to take with colchicine. It’s the preferred macrolide antibiotic when you need one while on colchicine.
What if I accidentally took clarithromycin with colchicine?
Stop the clarithromycin immediately and contact your doctor or go to the ER. Symptoms of toxicity can take 1-3 days to appear. Blood tests for kidney function, muscle enzymes (CK), and blood cell counts are critical. Colchicine levels can be checked in specialized labs, but treatment is based on symptoms, not just numbers.
Is this interaction only a problem for older people?
No. While older adults and those with kidney problems are at higher risk, cases have been reported in younger, otherwise healthy people. The interaction is dose- and time-dependent-not age-dependent. Even a single dose of clarithromycin can be dangerous if you’re on colchicine.
Are there other drugs besides macrolides that interact with colchicine?
Yes. Many drugs inhibit CYP3A4 or P-gp. These include diltiazem, verapamil, amiodarone, ketoconazole, itraconazole, ritonavir, ciclosporin, and even some statins like simvastatin. Always check with your pharmacist before starting any new medication, including over-the-counter ones.
Why isn’t this warning more widely known?
Because it’s complex. Colchicine is old, cheap, and widely used. Many doctors assume it’s harmless. Pharmacists may not be alerted if the system doesn’t flag it. Patients often don’t realize they’re on colchicine for heart issues, not gout. It’s a perfect storm of low awareness, poor EHR alerts, and the drug’s deceptive safety profile.






Lu Gao
31 January, 2026 . 23:42 PM
OMG I just realized my grandma was on colchicine and got clarithromycin last year 😱 She had that weird muscle pain and thought it was just "old age"-turns out she was almost in the ICU. Thank you for this post!! I’m telling everyone. 🙏❤️
Angel Fitzpatrick
1 February, 2026 . 11:08 AM
Let me guess-Big Pharma doesn’t want you to know this because azithromycin is cheaper and they make billions off the dangerous combo. CYP3A4? P-gp? These are just cover terms for the real agenda: controlling the masses with toxic pharmacology. The FDA’s database? Manipulated. The 147 cases? Underreported. They’re silencing the truth because they profit from your suffering. Wake up.
Nidhi Rajpara
3 February, 2026 . 05:26 AM
Dear author, I am writing from India where colchicine is sold over the counter without prescription. Many patients take it for joint pain without knowing its mechanism. This interaction is not just a concern-it is a public health emergency. I urge you to collaborate with Indian medical associations to spread awareness. Thank you for your meticulous research.
Chris & Kara Cutler
3 February, 2026 . 05:42 AM
THIS IS SO IMPORTANT!! 🚨 If you're on colchicine, DO NOT take clarithromycin. Switch to azithromycin. It’s that simple. Your muscles will thank you. Your kidneys will thank you. Your family will thank you. Share this. Now. 💪❤️
Rachel Liew
4 February, 2026 . 10:43 AM
I’m a nurse and I’ve seen this happen twice. One guy was 42, no kidney issues, just took clarithromycin for a sinus infection and ended up in the ER with rhabdo. He didn’t even know he was on colchicine for pericarditis. People think it’s just "gout medicine." It’s not. Please, if you’re reading this-ask your pharmacist. Seriously. It could save your life.
Lisa Rodriguez
5 February, 2026 . 06:07 AM
Wow this is eye-opening. I didn’t realize azithromycin was the safe one-I always thought all antibiotics were equal. I’m switching my dad’s script right now. Also, I just checked his meds-he’s on diltiazem too. So now I’m worried about that too. Anyone know if that’s a big risk with colchicine? I’ll ask his pharmacist tomorrow. Thanks for the heads up!
Lilliana Lowe
6 February, 2026 . 02:01 AM
While your post is factually accurate, it lacks the necessary scholarly rigor. You cite a 2022 study of 12,000 patients but omit the confidence interval. You reference FDA adverse events without clarifying underreporting bias. The EHR data from Epic? No peer-reviewed source cited. This is not medical education-it’s alarmist blogging dressed in clinical jargon. For true clinical insight, consult UpToDate or Micromedex-not Reddit.
Melissa Melville
7 February, 2026 . 03:38 AM
So let me get this straight-people are dying because they didn’t know that a $50 pill and a $10 antibiotic don’t play nice? And we’re surprised? Welcome to American healthcare, folks. Where you get a heart attack, then a pneumonia, then a coma-all because no one connected the dots. At least in my country, they just give you a shot and tell you to stop complaining.
Deep Rank
7 February, 2026 . 05:01 AM
Okay but let’s be real-this isn’t just about drugs, it’s about how we treat elderly people and the chronically ill. You think your grandma’s doctor really cares if she’s taking colchicine? No. He’s rushing between 30 patients. Pharmacies? They’re understaffed and automated. And patients? They’re too scared to ask questions. So we get this. We get death by bureaucracy. I’ve seen it. My aunt died like this. No one warned her. No one flagged it. The system failed. And now you’re just posting it like it’s news. It’s not news. It’s a crime.
Naomi Walsh
7 February, 2026 . 11:21 AM
As a clinical pharmacologist with 17 years in EU regulatory affairs, I must point out that your assertion about azithromycin being "almost no interaction" is misleading. The 2023 EMA review noted a minor P-gp inhibition at supratherapeutic doses. You’ve oversimplified a complex pharmacokinetic interaction for clickbait. This is dangerous. Patients deserve precision, not soundbites.
Bryan Coleman
8 February, 2026 . 11:51 AM
My doc switched me from clarithromycin to azithromycin last year after I mentioned I was on colchicine. I didn’t even know it was a thing. He was like, "Oh yeah, that’s a classic one." Like it’s common knowledge. Why isn’t this on every prescription screen? Anyway-glad I asked. Thanks for the post.
June Richards
9 February, 2026 . 10:10 AM
Why are we even talking about this? Just stop taking colchicine. It’s a toxic relic. There are better drugs now. If you’re still on it, you’re probably on Medicare and don’t know how to advocate for yourself. Just say no to ancient meds.
Jaden Green
10 February, 2026 . 21:39 PM
Colchicine? That’s what they gave my grandfather in the 80s. He died of multi-organ failure after a course of erythromycin. They never told us why. Now I read this and realize they didn’t know either. This isn’t a drug interaction-it’s a systemic failure of medical education. Every med student should be forced to memorize this one interaction before they touch a stethoscope. And EHRs? Still clueless. What a joke.
Donna Macaranas
11 February, 2026 . 03:19 AM
Thank you for writing this. I’ve been on colchicine for pericarditis since 2021 and just got a prescription for amoxicillin yesterday. I was about to take it without thinking-now I’m double-checking with my pharmacist. You saved me from a mistake I didn’t even know I was about to make. Small acts of awareness matter.
Jamie Allan Brown
12 February, 2026 . 09:42 AM
Just got off the phone with my cardiologist. He said if I ever need an antibiotic while on colchicine, azithromycin is the only safe option-and he’s now adding it to my med list in his notes. That’s the kind of change we need: not just awareness, but institutional action. Thank you for lighting the fire.