Most people don’t think about hepatitis B and C until someone they know gets sick. But these two viruses are quietly affecting millions worldwide-and many don’t even know they’re infected. Hepatitis B and C attack the liver, but they’re not the same. One has a vaccine. The other can be cured in eight weeks. Both can lead to liver cancer if left unchecked. Understanding how they spread, how to test for them, and what’s new in treatment isn’t just medical knowledge-it’s life-saving.
How Hepatitis B and C Spread-And What Doesn’t Spread Them
Hepatitis B is one of the most contagious viruses on the planet. It lives in blood and bodily fluids. You can catch it from sharing needles, having unprotected sex, or even from a mother to her baby during childbirth. In places like parts of Asia and Africa, up to 90% of chronic hepatitis B cases come from infections passed at birth. That’s why giving newborns the first dose of the hepatitis B vaccine within 24 hours is so critical. The World Health Organization says this simple step can cut mother-to-child transmission by over 95%. It’s not just needles and sex. The virus can survive on surfaces for at least seven days. That means sharing razors, toothbrushes, or even tattoo equipment with someone infected can put you at risk. But here’s what you don’t need to worry about: hugging, kissing, coughing, sharing food, or using the same toilet. Hepatitis B doesn’t spread through casual contact. Hepatitis C is different. It’s almost always spread through blood-to-blood contact. The biggest driver today? The opioid crisis. In the U.S., cases of acute hepatitis C jumped 71% between 2014 and 2018, mostly among people aged 20 to 39 who inject drugs. Needle sharing is the top cause. But it can also happen through unsterile medical equipment, tattoos done in unregulated settings, or even from mother to baby during pregnancy-though that’s less common, happening in about 5-6% of cases.Who Should Be Tested-and When
The CDC now recommends that every adult get tested for hepatitis C at least once in their lifetime. That’s a big shift from just testing high-risk groups. Why? Because nearly half of people with hepatitis C don’t know they have it. And without testing, they won’t get treated. That means the virus keeps spreading. For hepatitis B, testing is equally important. The CDC recommends all adults get screened once, but some groups need it more often: healthcare workers, people who inject drugs, men who have sex with men, people with HIV, and those born in countries where hepatitis B is common-like parts of Asia, Africa, Eastern Europe, and the Pacific Islands. Pregnant women should be tested for both viruses during every pregnancy. If a mother has hepatitis B, her baby can be protected with the vaccine and hepatitis B immune globulin right after birth. For hepatitis C, there’s no prevention at birth-but knowing the mother’s status helps doctors monitor the baby and catch infection early.Testing: What the Blood Tests Actually Tell You
Hepatitis B testing isn’t one test. It’s a panel. The first is HBsAg-this tells you if the virus is currently in your blood. If it’s positive, you’re infected. Then there’s anti-HBc, which shows you’ve been exposed at some point. Anti-HBs means you’re protected-either from vaccination or past infection. HBeAg and HBV DNA levels help doctors decide if you need treatment and how active the virus is. For hepatitis C, it’s simpler. First, an antibody test checks if your body has ever fought the virus. If it’s positive, you need a second test: HCV RNA. This tells you if the virus is still active in your blood. A lot of people test positive for antibodies but negative for RNA-meaning they cleared the virus on their own. That happens in about 25% of cases. New point-of-care tests are making this easier. The OraQuick HCV test gives results in 20 minutes. For hepatitis B, new rapid tests have over 98% accuracy in field studies. These tools are changing the game in rural clinics, homeless shelters, and drug treatment centers where people don’t have easy access to labs.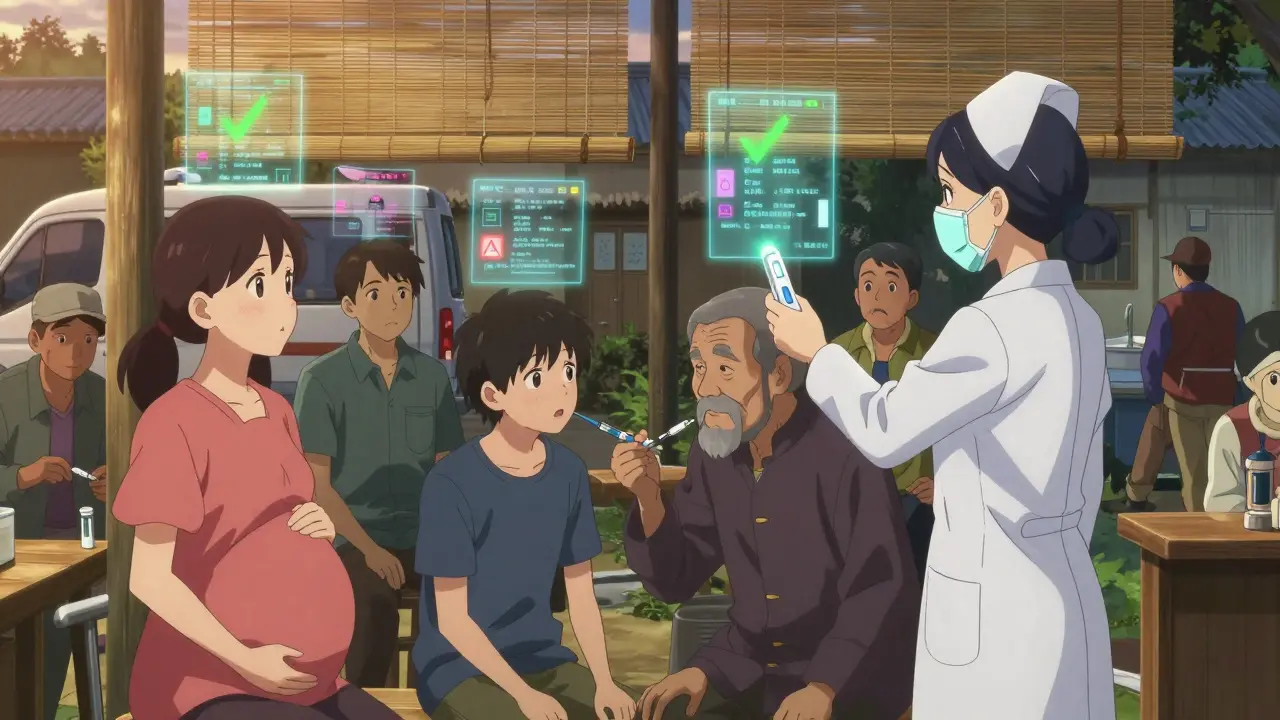
Treatment Advances: The Big Breakthroughs
Hepatitis C used to be a lifelong battle. In the 1990s, treatment meant weekly injections of interferon and daily pills for up to 48 weeks. Side effects were brutal: depression, fatigue, fever, and sometimes permanent damage. Cure rates? Around 40-50%. Then came direct-acting antivirals (DAAs). Drugs like sofosbuvir/velpatasvir (Epclusa) and glecaprevir/pibrentasvir (Mavyret) changed everything. These pills are taken daily for just 8 to 12 weeks. Side effects? Usually mild-headache or tiredness. Cure rates? Over 95% across all genotypes and patient types, even for those with cirrhosis or HIV co-infection. The cost used to be a barrier. In 2014, a full course of sofosbuvir cost $84,000. Today, generic versions cost under $300 in low-income countries. In the U.S., prices have dropped to $24,000-$30,000. Still, only 21% of people with hepatitis C got treated in 2020. Why? Lack of testing, stigma, and access issues in rural areas. Egypt’s story shows what’s possible. In 2014, 14.7% of Egyptians had hepatitis C. Through nationwide screening and low-cost treatment campaigns, that number dropped to 0.9% by 2021. That’s not science fiction-it’s public health done right.Hepatitis B: No Cure Yet, But Progress Is Happening
Unlike hepatitis C, hepatitis B can’t be cured yet. But it can be controlled. The goal is to stop the virus from damaging the liver. That’s done with antiviral pills like tenofovir alafenamide (TAF) and entecavir. These drugs suppress the virus so well that most people never develop cirrhosis or liver cancer. The catch? You usually have to take them for life. Stopping too soon can cause a dangerous rebound. Annual costs in the U.S. range from $6,000 to $12,000. That’s a barrier for many. But new hope is on the horizon. Researchers are testing drugs that target different parts of the virus. siRNA therapies like JNJ-3989 and capsid assembly modulators are in phase 3 trials. These aim to reduce or eliminate HBsAg-the protein that tells the immune system to ignore the virus. If they work, they could lead to a functional cure: where the virus stays gone even after stopping treatment. Right now, only 1-2% of people with chronic hepatitis B naturally clear HBsAg each year. That’s why a functional cure is the holy grail. Experts like Dr. Anna S. Lok say we’re closer than ever. Some patients in trials have already lost HBsAg after new treatments.
What’s Still Holding Us Back
We have the tools. But we’re not using them well. Hepatitis B vaccine coverage in U.S. adults is only 66.5%. The goal is 90%. Why the gap? Lack of awareness, vaccine hesitancy, and doctors not offering it. For hepatitis C, the problem isn’t the cure-it’s finding the people who need it. People who inject drugs, incarcerated individuals, and those without stable housing are hardest to reach. Community health workers have proven they can close this gap. In places like Kentucky and West Virginia, mobile clinics and peer-led outreach are increasing testing and treatment rates. The opioid crisis is still fueling new hepatitis C cases. In 2020, there were over 12,800 new acute infections in the U.S.-up from under 4,000 in 2010. Most were in rural areas. Without better access to clean needles, addiction treatment, and testing, this trend won’t reverse.What You Can Do Right Now
If you’ve never been tested for hepatitis B or C, get tested. It’s a simple blood draw. Most insurance covers it. If you’re uninsured, community health centers often offer free or low-cost screening. If you’re pregnant, ask for both tests. If you inject drugs, get tested every year. If you have a partner with either virus, get tested and talk about protection. If you’re eligible for the hepatitis B vaccine and haven’t had it, get all three doses. It’s safe, effective, and protects you for life. If you’ve been diagnosed with hepatitis C, talk to your doctor about DAAs. The cure is simple, short, and highly effective. Don’t wait. If you’re living with hepatitis B, stay on your meds. Get liver checks every six months. Avoid alcohol. Ask about new treatments in clinical trials. The tools to end hepatitis B and C as public health threats exist. What’s missing is action. Not tomorrow. Not next year. Now.Can you get hepatitis B from kissing or sharing food?
No. Hepatitis B is not spread through kissing, hugging, sharing meals, or using the same toilet. The virus is in blood and certain body fluids-like semen and vaginal fluids-but not in saliva, sweat, or tears. You can’t catch it from casual contact.
Is hepatitis C curable?
Yes. Hepatitis C is now curable in over 95% of cases with 8 to 12 weeks of oral antiviral pills. These drugs, called direct-acting antivirals (DAAs), have few side effects and work for all virus genotypes, even in people with liver scarring or HIV co-infection.
Can you get hepatitis B if you’ve been vaccinated?
The hepatitis B vaccine is 95% effective at preventing infection. If you completed the full 3-dose series, your protection lasts at least 20 years-and likely for life. You won’t get hepatitis B from the vaccine. It contains no live virus.
Do you need to be tested for hepatitis B if you’re vaccinated?
Usually not. If you were vaccinated as a child or adult and completed all doses, you’re protected. But if you’re a healthcare worker, have a partner with hepatitis B, or are immunocompromised, your doctor might check your antibody levels (anti-HBs) to confirm immunity.
Can hepatitis B turn into hepatitis C?
No. Hepatitis B and C are caused by completely different viruses. One doesn’t turn into the other. But someone can be infected with both at the same time-especially if they’ve had risky behaviors like needle sharing. Co-infection makes liver damage more likely, so testing for both is important.
Why is hepatitis B harder to cure than hepatitis C?
Hepatitis B hides in the liver as a stable DNA form called cccDNA, which current drugs can’t fully eliminate. Hepatitis C is an RNA virus that doesn’t integrate into human DNA. That’s why DAAs can wipe it out completely. For hepatitis B, scientists are working on new drugs to target cccDNA-but a cure isn’t available yet.
Is it safe to get pregnant if you have hepatitis B or C?
Yes. With proper care, you can have a healthy baby. If you have hepatitis B, your baby gets the vaccine and immune globulin within 12 hours of birth-this prevents infection in over 95% of cases. If you have hepatitis C, there’s a 5-6% chance of passing it to your baby, but no treatment is given during pregnancy. After birth, the baby is tested and monitored.




Paul Bear
11 January, 2026 . 03:09 AM
The hepatitis B vaccine is 95% effective, but only 66.5% of U.S. adults are vaccinated? That’s not just negligence-it’s a public health failure. We’ve had a safe, lifelong prophylactic since 1982, yet we treat it like a suggestion, not a standard of care. Healthcare providers need to stop asking if patients ‘want’ the vaccine and start prescribing it like they do for tetanus. The math is simple: 90% coverage is achievable. We’re not hitting it because we’ve normalized complacency.
And for hepatitis C, the 95% cure rate with DAAs is a miracle-but only if you can access it. The real crisis isn’t virology, it’s logistics. People aren’t dying from HCV; they’re dying from bureaucracy, stigma, and the assumption that ‘high-risk’ equals ‘deserving of neglect.’
Jaqueline santos bau
12 January, 2026 . 07:02 AM
Okay but can we talk about how WEIRD it is that people are terrified of sharing a toothbrush but will hug someone who just got out of prison with zero screening? I mean, come on. Hep B survives on surfaces for SEVEN DAYS. And yet we’re out here treating it like it’s the plague when it’s literally easier to prevent than the flu. And don’t even get me started on how we ignore people who inject drugs like they’re invisible. They’re not monsters-they’re humans with addiction. We could end HCV in five years if we stopped punishing people and started treating them.
Also, why is it still a thing that doctors don’t test pregnant women automatically? Like, is it really that hard to check a blood tube?
Aurora Memo
14 January, 2026 . 01:51 AM
I’ve worked in community health for over a decade, and I’ve seen the quiet devastation of undiagnosed hepatitis. One woman, 52, came in for fatigue-turned out she had cirrhosis from hepatitis C she’d had since the ’80s. Never tested. Never told. She thought it was just ‘bad luck.’
Testing should be routine, like cholesterol. No stigma. No judgment. Just care. And for those who are scared-know this: a simple blood draw can save your life, or your child’s. We don’t need more fear. We need more access. And we need to stop making people feel guilty for being sick.
Faith Edwards
15 January, 2026 . 11:47 AM
It is, frankly, an affront to the dignity of modern medicine that we continue to tolerate such abysmal rates of hepatitis B vaccination among adults in the United States. One is compelled to ask: if this were a vaccine for a sexually transmitted cancer caused by HPV, would we tolerate such lethargy? I think not. The conflation of hepatitis B with moral judgment-rather than epidemiological necessity-is not merely regressive, it is lethal.
Moreover, the persistence of needle-sharing as a vector for hepatitis C is not a consequence of individual failing, but of systemic abandonment. The opioid crisis is not a moral failure; it is a failure of social infrastructure. We have the pharmacological tools to eradicate HCV. What we lack is the political will to treat addiction as a medical condition rather than a criminal one.
Jay Amparo
17 January, 2026 . 07:40 AM
In India, we’ve seen how community health workers with simple rapid tests can change everything. In rural Bihar, we set up tents near bus stops and tested over 2,000 people in three weeks. Over 80 had hepatitis B. Half didn’t even know they were infected. We linked them to free clinics, and now they’re on treatment.
It’s not about fancy hospitals. It’s about showing up. And yes, the vaccine works. My cousin got all three doses at 14. Now she’s 32, a nurse, and never had a single needle stick scare. That’s the power of prevention.
Let’s stop waiting for someone to get sick. Let’s just test everyone. It’s not hard. It’s just… kind.
Lisa Cozad
19 January, 2026 . 00:41 AM
Just got tested yesterday-negative for both. Felt weird saying it out loud to the nurse. Like I was admitting something. But she just smiled and said, ‘Good job. You’re one of the few.’
Why does it feel like we’re supposed to be ashamed of getting tested? It’s not a confession. It’s a check-up. Like getting your tires rotated. I think we need to reframe this. Testing isn’t scary. Ignorance is.
Saumya Roy Chaudhuri
20 January, 2026 . 21:40 PM
Let me educate you. Hepatitis B is NOT just blood and sex. It’s also in saliva-just not enough to transmit unless there’s open wounds or bleeding gums. You think kissing is safe? Try deep kissing with gingivitis. I’ve seen cases. And hepatitis C? It’s not just needles. I had a patient who got it from a manicure tool. Unsterilized. In a salon. In Mumbai. So yes, you can get it from a pedicure. Don’t be naive. The CDC doesn’t list it because they don’t want to scare people. But I will.
Also, DAAs are expensive in the U.S. because Big Pharma owns the patents. In India, generics cost $20. You think that’s fair? No. It’s theft.
Mario Bros
21 January, 2026 . 01:21 AM
Just got my third Hep B shot last week 🙌
Worth every second. My buddy got liver cancer last year from it-didn’t even know he had it. Don’t be him. Get tested. Get vaccinated. Your future self will high-five you.
Also-yes, you can get cured of HCV. It’s not a death sentence. It’s a pill. Go ask your doc. Seriously.
Ritwik Bose
21 January, 2026 . 22:15 PM
The notion that hepatitis B and C are ‘silent killers’ is misleading. They are not silent-they are neglected. The silence comes from the absence of policy, from the absence of funding, from the absence of compassion. We have the tools. We have the knowledge. What we lack is the collective will to prioritize human life over cost-benefit analyses.
For hepatitis B, the cccDNA reservoir is indeed the central challenge. But let us not forget: the immune system is not inert. It is suppressed. The new siRNA therapies are not merely promising-they are revolutionary, because they restore immune recognition. This is not just treatment. This is immunological reawakening.
chandra tan
23 January, 2026 . 06:16 AM
In my village in Kerala, we used to say, ‘If your uncle has jaundice, don’t share his spoon.’ No one knew why, but we did it. Turns out, it was hepatitis B. We didn’t have tests. We had instinct.
Now, my niece got vaccinated at birth. No one in our family has it. That’s progress. Not magic. Just science. And it’s free at our public health center.
Don’t wait for someone to die before you act. Do the simple thing. Get tested. Get the shot. It’s not a favor. It’s your right.
Ted Conerly
23 January, 2026 . 21:25 PM
Let’s be clear: the hepatitis B vaccine is one of the most effective public health interventions in history. Yet we treat it like a bonus feature, not a baseline. Healthcare providers need to stop waiting for patients to ask. Start offering it like you offer flu shots. Universal screening for HCV? Done. Now let’s make universal vaccination for HBV just as normal.
And if you’re on antivirals for HBV? Don’t stop. Ever. The rebound risk isn’t theoretical-it’s deadly. Your liver doesn’t care if you’re ‘tired of pills.’ It only cares if you’re alive.
Dwayne Dickson
25 January, 2026 . 17:44 PM
Oh, so now we’re celebrating a 95% cure rate for hepatitis C like it’s some kind of miracle? Let’s not forget that this was achieved after decades of neglect, after thousands died because we prioritized profit over people. The fact that DAAs cost $30,000 in the U.S. while being $200 in Bangladesh isn’t a medical achievement-it’s a moral indictment.
And let’s not pretend that ‘testing everyone’ is a solution when the system can’t even handle the volume. We’ve got a cure, but we’ve got no infrastructure to deliver it. That’s not a health crisis. That’s a governance failure.
Michael Marchio
27 January, 2026 . 02:56 AM
It’s astonishing how many people still believe hepatitis B spreads through casual contact. I’ve had coworkers refuse to eat lunch with someone who tested positive, thinking they’d catch it from the shared salt shaker. This isn’t ignorance-it’s fear masquerading as logic. The virus is not airborne. It’s not in sweat. It’s not in tears. It’s in blood. And if you’re not bleeding into your coffee, you’re fine.
And yet, the stigma persists. People with HBV are denied jobs. Denied housing. Denied the right to be seen as human. We’ve cured the virus in the lab. But we haven’t cured the prejudice in the heart. That’s the real epidemic.
Ashlee Montgomery
28 January, 2026 . 11:17 AM
Tested. Negative. Got the vaccine. Done.