When you pick up a prescription, you might not realize that the pill in your hand wasn’t necessarily the one your doctor wrote on the paper. That’s because in most states, pharmacists are allowed-or even required-to swap your brand-name drug for a cheaper generic version. But here’s the catch: generic substitution laws aren’t the same in every state. Some states make it automatic. Others demand your permission. A few won’t let pharmacists substitute at all for certain drugs. This patchwork of rules affects your wallet, your safety, and how often you actually get the most affordable medication.
Why These Laws Exist
Generic drugs work the same way as brand-name drugs. They contain the same active ingredients, work the same way in your body, and are held to the same FDA standards. The only real difference? Price. Generics typically cost 80% to 85% less. In 2022, 90.7% of all prescriptions filled in the U.S. were for generics, saving patients and insurers billions. But without laws guiding when and how substitutions happen, pharmacists might not be able to switch your medication-even if it’s safe and cheaper.The first modern substitution law was passed in Louisiana in 1980. Since then, every state and Washington, D.C., has created its own rules. The goal? Cut costs without risking patient health. The FDA’s Orange Book is the official list that tells pharmacists which generics are considered therapeutically equivalent to brand-name drugs. But even if the FDA says two drugs are interchangeable, state laws can still block the swap.
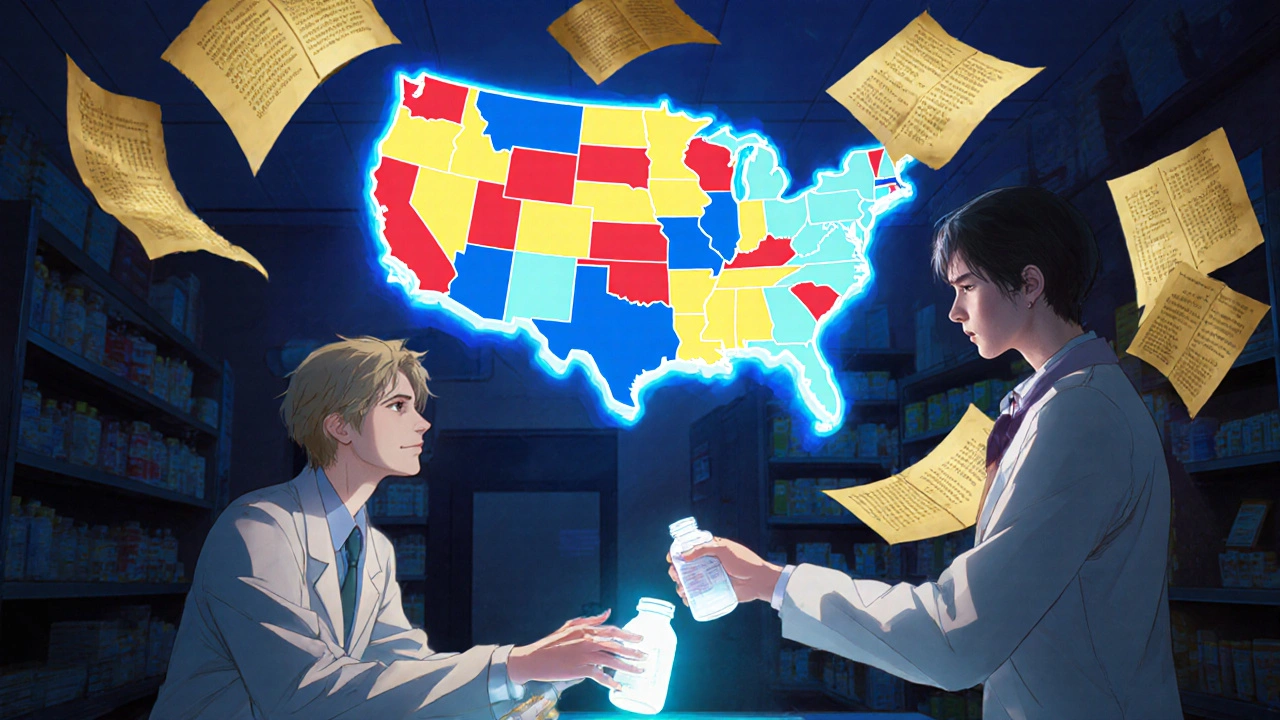
Mandatory vs. Permissive Substitution
There are two main types of laws: mandatory and permissive.In 19 states-including California, New York, and Texas-pharmacists must substitute a generic when it’s available, unless the doctor specifically says "do not substitute" (often written as "DAW 1" on the prescription). These states assume that if the FDA says it’s equivalent, then the pharmacist should use it. The result? Generic use in these states is 8 to 12 percentage points higher than in states with permissive laws. That means more savings for patients and insurers.
The other 31 states and D.C. use permissive laws. Here, pharmacists can substitute, but they don’t have to. Many choose to, especially if the patient has a low copay for the generic. But some pharmacists hesitate, especially if they’re unsure about the rules or worried about liability. In Alaska, Delaware, Maine, and New Hampshire, pharmacies are required to post signs saying substitution is possible. It’s a small step, but it gives patients a heads-up.
Who Gets to Say Yes or No? Patient Consent Rules
This is where things get messy. In seven states-Connecticut, Hawaii, Maine, Maryland, New Hampshire, Vermont, and West Virginia-plus Washington, D.C., the pharmacist must get your explicit consent before swapping your brand-name drug for a generic. That means they have to ask you, explain the difference, and get you to sign or say "yes" out loud.Why? Because some drugs have a narrow therapeutic index-tiny changes in dosage can cause big problems. Think of warfarin (a blood thinner), levothyroxine (for thyroid), or certain seizure medications. A slight difference in how your body absorbs the generic could mean your blood clots too easily or your seizures return.
Hawaii goes even further: it bans substitution of antiepileptic drugs unless both the doctor and the patient give consent. Kentucky has a list of drugs that can’t be substituted at all, including digitalis and some epilepsy meds. In Oklahoma, the pharmacist can’t substitute unless the prescriber or the patient gives permission. So even if the FDA says it’s safe, state law says no.
Notification After the Fact
Thirty-one states and D.C. don’t require consent before substitution-but they do require the pharmacist to notify you afterward. That means you get the generic, and then someone tells you: "We switched your medication."But here’s the problem: most patients don’t notice. A 2022 survey by the National Psoriasis Foundation found that 42% of patients on biologic medications didn’t know their drug had been swapped for a biosimilar-even though state laws required notification. Why? Because the notice often comes on a receipt, or in a phone call that gets ignored. Patients aren’t trained to read pharmacy fine print.

Liability: Who’s at Risk?
If something goes wrong after a substitution, who gets sued? In 24 states-including Alabama, Arizona, Illinois, Massachusetts, Missouri, Nebraska, New Mexico, Oregon, and Rhode Island-pharmacists have no legal protection from liability if a patient has a bad reaction after a generic is switched.That means pharmacists in those states may avoid substitutions out of fear, even when the FDA says it’s safe. One pharmacist in a multi-state chain told a Reddit community: "I have to check which state’s rules apply every time I fill a prescription for someone who lives near a border. It’s a nightmare." The National Community Pharmacists Association found that 68% of independent pharmacists spend 15 to 30 minutes a day just managing substitution paperwork and legal questions.
Biologics and Biosimilars: A New Layer of Complexity
Biologics are complex drugs made from living cells-used for conditions like rheumatoid arthritis, Crohn’s disease, and cancer. They’re expensive. Biosimilars are cheaper versions that are "highly similar" to the original, but not identical.Forty-five states treat biosimilars differently than regular generics. They require stricter rules: the FDA must first designate the biosimilar as "interchangeable," and pharmacists must notify the prescribing doctor within 2 to 7 days after swapping. Six states that require generic substitution still treat biosimilars as optional. That means a patient on a brand-name biologic might get a cheaper biosimilar in one state but not in another-even if the FDA says it’s safe.
As of 2023, biosimilars made up only 11.2% of all biologic prescriptions. One reason? Confusion. Patients don’t understand the difference. Pharmacists don’t know the rules. Doctors don’t always approve the switch.
How Technology Is Helping (and Hurting)
Electronic health records now include "State Substitution Rules Engines" that automatically apply the right law based on the pharmacy’s location. Epic Systems, one of the biggest EHR providers, says their system reduced substitution errors by 37% after launching the tool in 2019.But not every pharmacy uses the same system. Independent pharmacies often rely on paper lists or outdated apps. The FDA’s Orange Book app gives real-time equivalence ratings, but many pharmacists still use printed guides. And in states with complex rules-like those requiring consent for certain drugs-manual checks still dominate.

What’s Changing in 2025?
In 2023, 12 states introduced bills to standardize substitution laws. The goal? Create a common set of rules so pharmacists don’t have to memorize 51 different sets of instructions. The FDA also updated the Orange Book in 2022 to include new "interchangeability" labels for complex generics. Eighteen states are reviewing their laws as a result.Research shows that when states simplify their rules-especially by removing consent requirements-generic use jumps. One 2023 study found that states that cut red tape saw generic utilization rise by 6.8 percentage points on average. In states that removed consent entirely, the jump was 11.2 points.
Still, the Congressional Budget Office estimates that without nationwide standardization, the U.S. will waste $4.7 billion a year on unnecessary brand-name prescriptions by 2030. That’s money that could go toward care, not profit margins.
What This Means for You
If you take a chronic medication-especially for epilepsy, thyroid disease, heart conditions, or autoimmune disorders-know your state’s rules. Ask your pharmacist: "Can you substitute this? Do I need to give permission?" Check your prescription label. If your drug switched without warning, you have a right to ask why.Medicaid programs in 42 states already force generic substitution and offer lower copays for generics. But in private insurance, it’s still a lottery. Your pharmacy might be in a permissive state, but your doctor’s office might be in a mandatory one. The system isn’t broken-it’s just messy.
The bottom line: generic substitution laws are designed to save money and improve access. But when they’re inconsistent, they create confusion, delay care, and sometimes cost more in the long run. Standardization isn’t just a policy goal-it’s a patient safety issue.
Can my pharmacist switch my brand-name drug without telling me?
It depends on your state. In 31 states and Washington, D.C., pharmacists must notify you after swapping your medication. In 7 states plus D.C., they must get your consent before switching. In the remaining states, they can substitute without asking-but many still inform patients as a best practice. Always check your prescription label and receipt for changes.
Are generic drugs really as safe as brand-name ones?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove they work the same way in the body. The only differences are in inactive ingredients like fillers or dyes, which rarely cause issues. For most people, generics are just as safe and effective.
Why are some drugs, like epilepsy meds, excluded from substitution?
Drugs with a narrow therapeutic index-like levothyroxine, warfarin, and certain antiseizure medications-have very little room for error. Even small differences in how your body absorbs the generic version could lead to serious side effects. That’s why states like Kentucky, Hawaii, and others specifically ban substitution for these drugs unless both the doctor and patient agree.
Can I refuse a generic substitution if my pharmacist offers it?
Yes. Even in states where substitution is mandatory, you can always say no. You have the right to request the brand-name drug. Your pharmacist may need to call your doctor to confirm, and you might pay more out of pocket-but your choice comes first.
How do I find out what my state’s substitution law is?
The National Association of Boards of Pharmacy offers a free, interactive map that updates quarterly with each state’s current substitution rules. You can also ask your pharmacist directly or check your state’s board of pharmacy website. If you’re unsure, it’s always okay to ask: "What are the rules here for switching my medication?"
Do biosimilars follow the same rules as regular generics?
No. Biosimilars are more complex and are treated differently. Most states require the FDA to label them as "interchangeable" before substitution is allowed. Pharmacists must notify the prescribing doctor within days of switching, and many states require patient consent. These extra steps are why biosimilars make up less than 12% of biologic prescriptions, even though they’re cheaper.
What to Do Next
If you take a chronic medication, especially one with a narrow therapeutic index:- Ask your pharmacist what your state’s substitution rules are.
- Check your prescription label every time you refill.
- If your drug changed without warning, call your doctor and ask if it’s safe.
- Use the FDA’s Orange Book app to verify therapeutic equivalence.
- Consider asking your doctor to write "Do Not Substitute" on your prescription if you’ve had issues before.
Generic substitution laws are meant to help you save money. But only if you understand them. Don’t assume the system works the same everywhere. Know your rights. Ask questions. And never hesitate to speak up if something doesn’t feel right.



Douglas Fisher
27 November, 2025 . 14:30 PM
Wow, I had no idea how wildly different the rules are between states-like, in New York, they just swap it out, but in Hawaii, you need a signed consent form just to get a thyroid med? That’s insane. I’ve had my levothyroxine switched without warning before, and I didn’t even notice until my heart started racing… Then I checked the bottle. I’m never trusting a pharmacy receipt again. Always double-check the label. Always. Always. Always.
Albert Guasch
29 November, 2025 . 04:45 AM
The current regulatory architecture governing pharmaceutical substitution is predicated upon a fragmented federalism model, wherein state boards of pharmacy exercise autonomous jurisdiction over therapeutic equivalence protocols. This results in suboptimal patient outcomes due to cognitive dissonance between FDA-established bioequivalence standards and state-mandated consent requirements. A unified, nationally standardized framework-modeled after the Uniform Prescription Drug Substitution Act-is imperative to mitigate liability exposure, reduce administrative burden on community pharmacists, and enhance cost-containment efficacy without compromising clinical safety.
Vanessa Carpenter
30 November, 2025 . 09:31 AM
It’s wild how much this affects people without them even knowing. I used to work at a pharmacy in Ohio-we had to notify people after the switch, but most just shrugged and walked out. One lady came back three days later because her anxiety got worse. Turns out they swapped her seizure med without her realizing. She didn’t even know it was a different brand. We’re saving money, sure… but at what cost?
Bea Rose
1 December, 2025 . 06:31 AM
Biologics aren't generics. Stop pretending they are. The FDA’s "interchangeable" label is marketing, not science. Biosimilars have structural variations that affect immunogenicity. States requiring physician notification are the only ones doing their job. The rest are gambling with lives.
Michael Collier
1 December, 2025 . 11:37 AM
It is imperative to recognize that the current state-by-state regulatory variance introduces significant inefficiencies into the healthcare delivery system. The National Association of Boards of Pharmacy’s interactive map, while useful, is not sufficient. A federal baseline standard, aligned with FDA interchangeability criteria, should be enacted to ensure equitable access, reduce pharmacist liability exposure, and eliminate the administrative burden that currently consumes 15–30 minutes per prescription. Patient safety and cost savings are not mutually exclusive objectives.
Shannon Amos
2 December, 2025 . 17:26 PM
So let me get this straight… I can get my $15 generic blood pressure pill without asking, but if I’m on a $5,000 biologic for my rheumatoid arthritis, I need a goddamn seminar and a notary? What even is this? My insurance doesn’t care how much it costs me, as long as it’s not their brand.
stephen riyo
4 December, 2025 . 06:11 AM
I’ve been filling scripts for 18 years, and I still get confused-especially with patients who live near state borders. One guy comes in from Indiana, gets his warfarin swapped in Ohio, then goes home to Kentucky and his INR goes through the roof. I’ve had pharmacists cry over this stuff. We’re not lawyers. We’re not doctors. We’re just trying to get people their meds without getting sued. Why can’t the feds just make one rule?
Wendy Edwards
5 December, 2025 . 14:47 PM
ok so i just got my levothyroxine switched and i felt like a zombie for a week. i thought it was stress. turns out the generic had a different filler and my body hated it. i told my doc and now he writes "do not substitute" on everything. i don’t care if it costs 20 bucks more. i’d rather pay than feel like i’m dying every day. also why is it that the people who make these rules never take these meds? just saying.
Jaspreet Kaur
7 December, 2025 . 12:16 PM
The system is not broken-it is a mirror. We demand cheap medicine but fear change. We trust science until it asks us to adapt. Generics are not inferior-they are the people’s medicine. Yet we cling to brand names like security blankets. Perhaps the real issue is not law or liability-but our fear of simplicity. Let the market work. Let the pharmacist dispense. Let the patient decide. Trust is the missing ingredient-not more regulation.