Levothyroxine-PPI Dose Adjustment Calculator
Medication Information
According to the article, proton pump inhibitors (PPIs) raise stomach pH, which can reduce levothyroxine absorption by up to 25%. This typically requires dose adjustments when both medications are taken together.
Studies show that patients taking both drugs often need a 12.5-25 mcg increase in levothyroxine dose to maintain stable thyroid function.
Important: This calculator provides an estimate based on clinical data. Always consult your healthcare provider before making any medication adjustments.
Input Your Current Information
Results
Based on your TSH:
Estimated adjustment needed:
New recommended dose:
According to clinical studies, TSH levels above 4.5 mIU/L typically require dose adjustment when taking PPIs. The adjustment amount is based on the difference between your current TSH and the upper limit of normal.
When you take levothyroxine every morning to manage hypothyroidism, you expect it to work. But if you're also taking a proton pump inhibitor (PPI) for heartburn or acid reflux, your thyroid medication might not be absorbing properly-even if you're following all the rules. This isn't speculation. It's a well-documented interaction that affects nearly 2.7 million Americans taking both drugs, according to IQVIA data from 2022. And the consequences? Fatigue, weight gain, and unexplained rises in TSH levels that make your endocrinologist scratch their head.
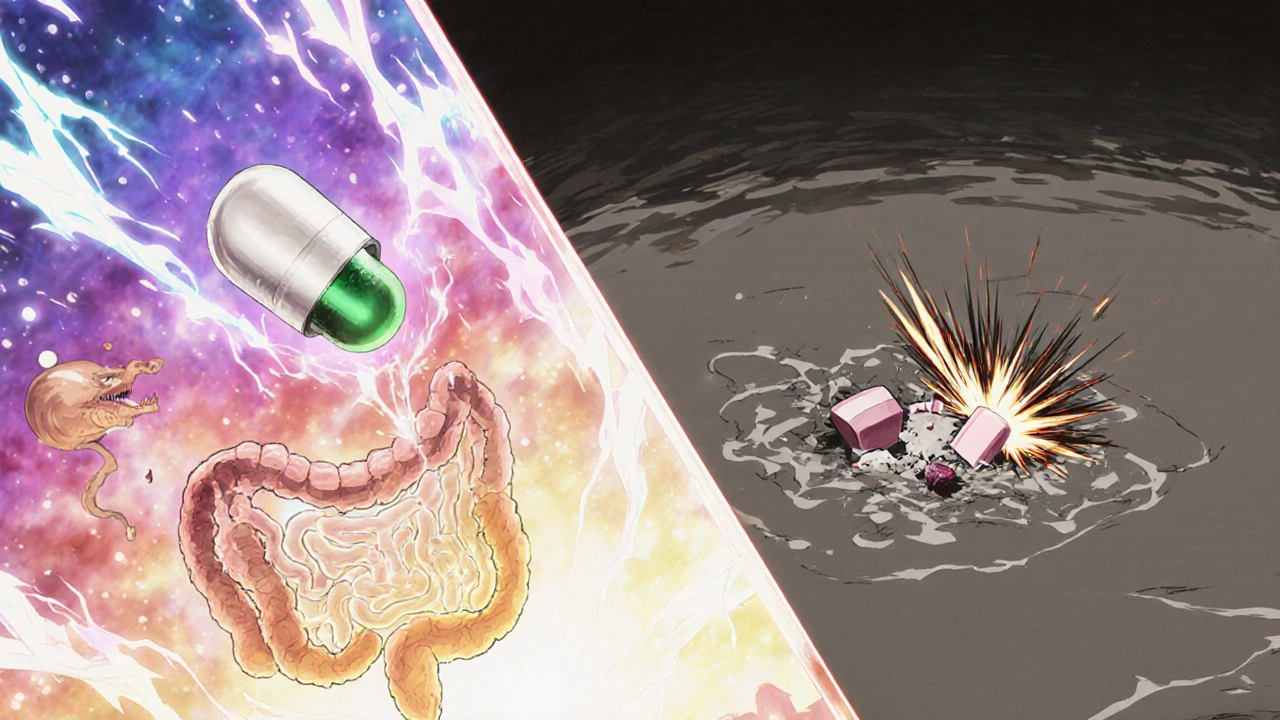
Why Levothyroxine Needs Acid
Levothyroxine isn't like most pills. It doesn't just dissolve and get absorbed. It needs an acidic environment in your stomach to break down and enter your bloodstream. That’s why doctors tell you to take it on an empty stomach, at least 30 to 60 minutes before breakfast. The ideal stomach pH for levothyroxine absorption is between 1 and 2-highly acidic, like vinegar. Proton pump inhibitors (PPIs) like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) shut down your stomach’s acid production. They block the H+/K+ ATPase enzyme in gastric cells, which is what pumps acid into your stomach. After taking a PPI, your stomach pH can rise to 4-6. That’s not just a little less acidic. It’s the difference between lemon juice and tap water. A 2021 systematic review in the Journal of General Internal Medicine analyzed seven studies and found that when people took PPIs with levothyroxine, their TSH levels rose significantly. Higher TSH means your thyroid isn’t getting enough hormone. That’s the body’s alarm bell telling you your levothyroxine isn’t working as it should.What the Studies Show
One 2023 study published in PubMed (PMID: 37259094) followed patients already stable on levothyroxine who started taking 40mg of pantoprazole daily. After just six weeks, their TSH levels jumped-even when they took the PPI at night, 30 minutes before dinner. That’s important. Many people think separating the doses by hours will fix the problem. But the study showed it didn’t matter if they took them together or hours apart. The PPI was still suppressing acid for up to 72 hours. Timing doesn’t rescue absorption. Another analysis from Mayo Clinic Proceedings (2020) found that 15-20% of patients on both drugs needed a levothyroxine dose increase. The average increase? 12.5 to 25 micrograms per day. That’s not a small tweak. It’s the difference between 75 mcg and 100 mcg-a jump that can throw off your entire hormone balance if not monitored.Who’s Most at Risk?
You’re more likely to run into this problem if:- You’ve been on a PPI for more than 3 months
- You’re over 65
- You take levothyroxine with food or coffee
- You have Hashimoto’s thyroiditis and are already sensitive to small changes in hormone levels
What Can You Do?
There are three solid options if you’re on both medications.1. Switch to Liquid Levothyroxine
Tirosint-SOL is a liquid form of levothyroxine that doesn’t need stomach acid to absorb. It’s made with glycerin instead of fillers that rely on acidity. A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed it works just fine even with PPIs. The catch? It costs $350 a month. Generic tablets are $15-$25. Insurance often won’t cover the liquid version unless you’ve tried and failed with tablets. But for some people, the price is worth it-especially if they’ve struggled with symptoms for years.2. Switch from PPIs to H2 Blockers
Famotidine (Pepcid) is an H2 receptor antagonist. It reduces acid too, but not as deeply or as long-lasting as PPIs. A 2018 study in Pharmacotherapy found no significant change in TSH levels when patients took famotidine with levothyroxine. If you only need acid relief a few times a week, this might be a better fit. But if you have severe GERD or Barrett’s esophagus, PPIs are still more effective. It’s a trade-off: less control over acid vs. better thyroid absorption.3. Monitor and Adjust Dose
If you can’t stop the PPI-for example, if you’re on it for a stomach ulcer or to prevent NSAID damage-you’ll need to monitor your TSH. The American Association of Clinical Endocrinologists recommends:- Check your TSH before starting the PPI
- Test again at 6-8 weeks after starting it
- If TSH is above your target range, increase levothyroxine by 12.5-25 mcg
- Recheck TSH in 6-8 weeks
What Doesn’t Work
Don’t waste time trying to separate doses. Taking levothyroxine at 6 a.m. and the PPI at 8 p.m. won’t help. PPIs don’t wear off after a few hours. Their effect lasts 24-72 hours, depending on the drug. Even if you take them 12 hours apart, your stomach is still too neutral for levothyroxine to absorb properly. Also, avoid taking levothyroxine with calcium, iron, or soy products. These interfere too. But that’s a separate issue. The PPI interaction is different-it’s about pH, not binding.
What’s Coming Next
The FDA is working on new labeling guidelines for thyroid medications that will clearly warn about PPI interactions. That’s a big step. Right now, many doctors don’t know this interaction exists-or they think timing fixes it. Researchers are also testing enteric-coated levothyroxine tablets designed to dissolve in the small intestine, not the stomach. These could bypass the acid problem entirely. Phase 3 trials (NCT04892357) are ongoing. If they work, we could have a new standard by 2027. And there’s another development: Tirosint-SOL’s patent expires in 2025. That means generic versions could hit the market, possibly dropping the price from $350 to under $50 a month. That would change everything for patients stuck between acid reflux and fatigue.What You Should Do Today
If you’re taking levothyroxine and a PPI:- Don’t panic. This is common and fixable.
- Check your last TSH result. If it’s been more than 3 months, ask your doctor for a test.
- Write down how you feel. Fatigue? Weight gain? Brain fog? Bring it to your appointment.
- Ask: “Could my PPI be affecting my thyroid meds?”
- Don’t stop your PPI on your own. Talk to your doctor about alternatives.
Can I take levothyroxine and a PPI at the same time?
No, taking them together reduces levothyroxine absorption. But even separating them by hours won’t fix the problem because PPIs suppress acid for up to 72 hours. The best solutions are switching to liquid levothyroxine, using an H2 blocker like famotidine, or adjusting your levothyroxine dose under medical supervision.
How do I know if my levothyroxine isn’t working because of my PPI?
If you’ve recently started a PPI and notice new or worsening fatigue, weight gain, cold sensitivity, or brain fog, your TSH may be rising. A blood test is the only way to confirm. If your TSH increases by more than 2-3 mIU/L after starting a PPI, it’s likely the interaction is affecting your absorption.
Is Tirosint-SOL worth the cost?
For patients who’ve tried multiple dose adjustments and still have symptoms, yes. Tirosint-SOL absorbs reliably even with PPIs, eliminating the guesswork. At $350/month, it’s expensive-but if you’re spending $100/month on doctor visits, blood tests, and extra meds because your thyroid isn’t stable, it may pay for itself. Generic levothyroxine will be available after 2025, which could drop the price significantly.
Can I switch from a PPI to famotidine?
Yes, if your acid reflux is mild to moderate. Famotidine (Pepcid) doesn’t suppress acid as deeply as PPIs, but studies show it doesn’t interfere with levothyroxine absorption. If you have severe GERD, Barrett’s esophagus, or a history of ulcers, your doctor may still recommend a PPI. But for many, famotidine taken as needed is a safer alternative for thyroid patients.
How often should I get my TSH checked if I’m on both drugs?
Get tested before starting the PPI, then again at 6-8 weeks after starting it. If your dose changes, recheck in another 6-8 weeks. Once stable, annual checks are usually enough-but if you change your PPI dose or switch medications, test again. Many patients stabilize within 12 weeks after a levothyroxine adjustment.






Jeff Moeller
19 November, 2025 . 10:34 AM
PPIs are just lazy medicine. We used to fix acid with diet and time, not chemical shutdowns. Now we got a whole generation on proton blockers like they're vitamins. And yeah, it kills levothyroxine. But who's really to blame? The drug companies selling the fix, or the doctors who never asked why you needed it in the first place?
Herbert Scheffknecht
20 November, 2025 . 05:29 AM
Think about it this way - your stomach isn't just a chemical reactor, it's a philosopher. It knows when to be angry, when to be calm. PPIs don't just reduce acid, they silence the conversation. And levothyroxine? It's just trying to get through the door. No wonder it's confused. We treat biology like a machine you can tweak with buttons. But bodies aren't code. They're poetry written in pH.
Jessica Engelhardt
21 November, 2025 . 09:16 AM
I've been on Nexium for 8 years and my TSH was fine until last year. Then I switched to Tirosint and boom - energy like I'm 25 again. Who cares if it's expensive? My job is draining me, my kids need their mom functional, and my doctor didn't even mention this interaction until I brought it up. America's healthcare system is broken but this? This is the one thing I can fix myself.
prasad gali
22 November, 2025 . 07:30 AM
The data is clear. PPI-induced hypothyroidism is underdiagnosed. The 2021 JGIM meta-analysis showed pooled effect size of 1.82 (95% CI 1.45–2.21) for TSH elevation. And the Mayo Clinic study? 18.7% average dose escalation. This isn't anecdotal. It's pharmacokinetic reality. Stop blaming patients. Start screening.
Paige Basford
23 November, 2025 . 12:25 PM
I actually tried famotidine after reading this and it worked great for my heartburn! I only take it 2-3 times a week now. My TSH stayed stable. I also started taking my levothyroxine with water only - no coffee, no food, no supplements. Small changes, big difference. My endo was impressed. You don't need to be perfect, just consistent.
Ankita Sinha
25 November, 2025 . 07:42 AM
OMG I JUST REALIZED THIS IS WHY I'VE BEEN SO TIRED!! I'm on omeprazole and levothyroxine and I thought it was just stress or bad sleep. I'm booking a blood test tomorrow. Also, I've been taking my pill with my morning coffee - no wonder. I'm switching to water and waiting 45 mins. Thank you for this post. You just saved my life 🙏
Kenneth Meyer
26 November, 2025 . 20:22 PM
The real issue isn't the interaction. It's that we treat thyroid disease like a dial you turn. TSH is a proxy, not a target. Some people need higher TSH to feel normal. Some need lower. But the system demands a number. So we keep adjusting doses without asking how the person feels. The PPI just exposes the flaw. The problem was always the metric.
Donald Sanchez
27 November, 2025 . 14:04 PM
Bro I was on 100mcg for 2 years then started omeprazole and my TSH jumped to 8.5. I thought I was going crazy. Then I found this thread. Switched to Tirosint-SOL and now I'm at 75mcg and feel like a new person. Also I use emojis now because why not 🤯💊📉📈. My doc didn't even know this was a thing. Google is my endo now.
Abdula'aziz Muhammad Nasir
27 November, 2025 . 22:10 PM
This is an excellent summary. For those in developing regions where Tirosint-SOL is inaccessible, the key is consistent monitoring. Even in Nigeria, where access to endocrinology is limited, basic TSH testing is available in most urban clinics. If you are on long-term PPI therapy, request a baseline and follow-up test. Your thyroid health is worth the effort. Do not delay. Your body speaks - listen.