Serotonin Syndrome Risk Calculator
Risk Assessment Tool
This tool helps healthcare providers assess the risk of serotonin syndrome when linezolid is combined with antidepressants based on key clinical factors.
Risk Assessment Result
Linezolid is a powerful antibiotic used for tough infections like MRSA and VRE-bugs that don’t respond to regular antibiotics. But there’s a quiet danger lurking in its chemistry: it can interfere with how your brain handles serotonin. When taken with antidepressants, this interaction can, in rare cases, trigger serotonin syndrome, a serious and sometimes deadly condition.
What is serotonin syndrome?
Serotonin syndrome isn’t just feeling a little off. It’s a medical emergency caused by too much serotonin in your nervous system. Think of serotonin as your brain’s natural mood and nerve signal chemical. When levels spike, your body goes into overdrive.
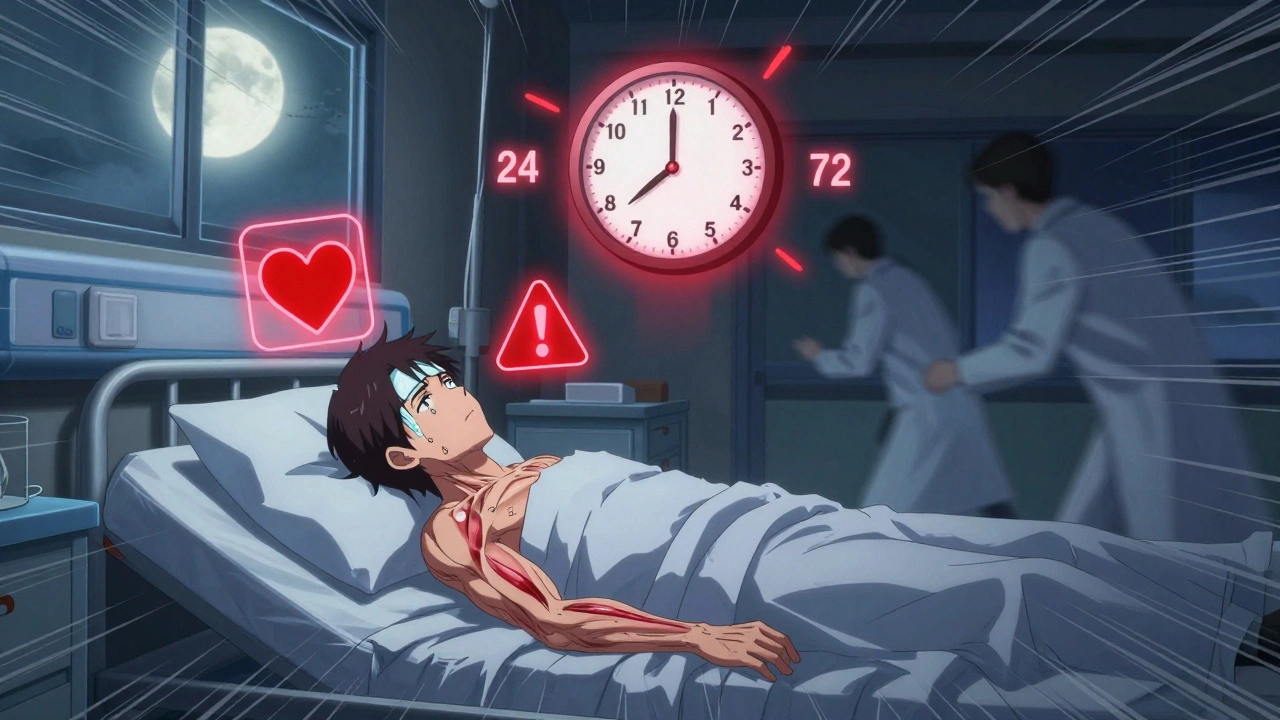
The classic signs show up in three areas:
- Cognitive: Agitation, confusion, restlessness, hallucinations
- Autonomic: Sweating, rapid heartbeat, high blood pressure, fever (sometimes over 104°F)
- Neuromuscular: Shaking, muscle stiffness, twitching, overactive reflexes, loss of coordination
In severe cases, it can lead to seizures, kidney failure from muscle breakdown (rhabdomyolysis), or even death. Symptoms usually appear within 24 to 72 hours after starting or increasing a drug that boosts serotonin. The faster you spot them, the better your chances of recovery.
How does linezolid cause this?
Linezolid was originally designed as a psychiatric drug. It was found to mildly block monoamine oxidase (MAO), the enzyme that breaks down serotonin. Even though it’s now used as an antibiotic, that old mechanism is still active.
Most antidepressants-like SSRIs (fluoxetine, sertraline), SNRIs (venlafaxine, duloxetine), and even older MAO inhibitors (phenelzine)-also raise serotonin levels. When you combine them with linezolid, you’re essentially double-pumping serotonin into your system. Your body can’t clear it fast enough.
Here’s the twist: linezolid isn’t as strong as the classic MAO inhibitors used for depression. Its MAO-blocking power is about 50 times weaker. That’s why serotonin syndrome is rare-but not impossible.
Is the risk actually high?
For years, doctors were told to avoid linezolid entirely if a patient was on any antidepressant. The FDA issued a warning in 2011 after a handful of serious cases. But recent data tells a different story.
A 2023 study in JAMA Network Open followed over 1,100 patients taking linezolid. Nearly 20% of them were also on antidepressants. Shockingly, serotonin syndrome occurred in fewer than 0.5% of all patients-and even fewer in those taking antidepressants. In fact, the risk was slightly lower in the antidepressant group. The researchers concluded: “Linezolid is likely safe for patients receiving antidepressants.”
A 2024 study of nearly 4,000 patients confirmed this: no significant increase in serotonin syndrome risk when linezolid and antidepressants were used together.
So why the warning? Because isolated cases still happen. One 70-year-old woman developed full-blown serotonin syndrome on linezolid alone-no antidepressants. Another patient on high-dose linezolid (600 mg twice daily) and multiple serotonergic drugs ended up in intensive care. The problem isn’t the combo itself-it’s the perfect storm of risk factors.
Who’s at real risk?
Not everyone is equally vulnerable. The real danger comes from:
- High doses of linezolid: 600 mg twice daily (used for serious infections) carries more risk than the standard 600 mg once daily.
- Multiple serotonergic drugs: Taking linezolid with an SSRI and tramadol and dextromethorphan? That’s a recipe for trouble.
- Older adults: Aging slows drug metabolism. People over 70 are more sensitive to CNS effects.
- Kidney problems: Linezolid is cleared by the kidneys. If they’re not working well, the drug builds up.
- History of serotonin syndrome: If it happened before, it can happen again.
Even herbal supplements like St. John’s wort or ginseng can add to the risk. So can certain pain meds like meperidine or fentanyl, and migraine drugs like sumatriptan.
What should doctors and patients do?
The guidelines are mixed. The Infectious Diseases Society of America says you can use linezolid with SSRIs if you monitor closely. The American Psychiatric Association still lists it as a “moderate risk.” The FDA hasn’t changed its warning since 2011.
Here’s what works in real practice:
- Don’t automatically avoid it. If you need linezolid for a life-threatening infection, don’t delay treatment because of fear.
- Check the full med list. Ask about every pill, patch, supplement, and OTC drug the patient takes. Don’t forget cough syrups and migraine meds.
- Start low, monitor daily. Use the lowest effective dose of linezolid. Watch for symptoms every day-especially in the first 3 days.
- Know the red flags. If someone suddenly becomes confused, sweaty, and shaky after starting linezolid, suspect serotonin syndrome.
- Stop linezolid immediately. If symptoms appear, get rid of the drug. Don’t wait.
Treatment is straightforward: stop the offending drugs, give benzodiazepines for agitation and muscle stiffness, use cyproheptadine (a serotonin blocker) if needed, and cool the body if there’s a fever. Most people recover within 24 hours if treated early.

What about food?
You’ve probably heard that MAO inhibitors mean no aged cheese or cured meats. That’s true for strong MAOIs like phenelzine. But linezolid? The risk is minimal. You don’t need to go on a strict diet. Still, if you’re on high-dose linezolid and eat a giant plate of blue cheese and salami, you might feel a bit off. It’s not a major concern, but be aware.
Bottom line: It’s rare, but you still need to be smart
Linezolid is a lifesaver for drug-resistant infections. The fear of serotonin syndrome shouldn’t stop you from using it when needed. The evidence now shows that combining it with antidepressants is far safer than we once thought.
But safety isn’t about avoiding risk-it’s about managing it. Know your patient’s meds. Watch for symptoms. Don’t assume the worst, but don’t ignore the signs. Most patients will be fine. A few won’t-and those are the ones you need to catch early.
If you’re on an antidepressant and your doctor prescribes linezolid, ask: “Is this the best option? What should I watch for?” You’re not being difficult-you’re being smart.
What if I’m already on linezolid and an antidepressant?
If you’re already taking both and feel fine, keep going. Don’t stop either without talking to your doctor. The risk is low. But if you notice any new symptoms-especially agitation, sweating, tremors, or a sudden fever-call your provider immediately. Don’t wait. Serotonin syndrome gets worse fast.




Saket Modi
3 December, 2025 . 04:46 AM
Bro just skip linezolid entirely. I got prescribed it last year and my brain felt like it was melting. 🤯 Stay safe.
Chris Wallace
3 December, 2025 . 19:56 PM
I’ve been on sertraline for 8 years and just finished a 10-day course of linezolid for a stubborn staph infection. No issues. I monitored myself like a hawk-checked my pulse, watched for sweating, avoided extra caffeine-but honestly? I felt fine. The fear around this interaction feels way overblown, especially since the JAMA study came out. Maybe we’ve been treating patients like they’re fragile glass since the 2011 FDA warning, when the real risk is closer to lottery-ticket levels. Not saying ignore it-but don’t let outdated guidelines scare you out of life-saving antibiotics.
william tao
5 December, 2025 . 00:14 AM
The assertion that linezolid is 'likely safe' is an egregious oversimplification. The pharmacokinetic interplay between monoamine oxidase inhibition and serotonergic agents is not a binary variable; it is a dynamic, dose-dependent, and patient-specific phenomenon. To dismiss the FDA's warning as obsolete is to ignore the very foundation of clinical pharmacology: individual variability. One case of serotonin syndrome is one too many.
Sandi Allen
5 December, 2025 . 08:28 AM
I knew it!! I KNEW IT!! They’re hiding the truth again!! Linezolid is a BIG PHARMA Trojan horse!! They want us on antidepressants AND antibiotics so we stay dependent!! Look at the study-only 1,100 patients?? That’s nothing!! What about the ones who died and weren’t counted?? And what about the elderly?? They’re being experimented on!! I read a guy on a forum who got seizures after just 3 days!! THEY DON’T WANT YOU TO KNOW THIS!!
John Webber
6 December, 2025 . 06:07 AM
i read this article and i think its kinda right but also kinda not? like if you take like 2 or 3 serotonergic things at once with linezolid you probs gonna have a bad time. i had a friend who took tramadol and zoloft and then got linezolid and he was all shaky and confused. he went to er. so yeah. just be careful. dont be dumb.
Shubham Pandey
7 December, 2025 . 12:14 PM
Linezolid + SSRI = fine. Just don’t be dumb with extra meds.
Elizabeth Farrell
8 December, 2025 . 17:09 PM
I want to say thank you for writing this so clearly. As someone who’s had to explain to my elderly mother why she can’t just stop her antidepressants when she gets an infection, this is the kind of balanced, compassionate information that’s so rare. You’re right-fear shouldn’t delay treatment, but awareness should guide it. I’ve shared this with my family and my nurse practitioner. The way you laid out the red flags and the ‘what to do’ steps? That’s the kind of guidance that saves lives without causing panic. You’ve done good work here.
Sheryl Lynn
9 December, 2025 . 13:08 PM
Ah yes, the classic 'evidence-based medicine' rebranding of pharmacological recklessness. Linezolid’s MAO inhibition may be '50 times weaker' than phenelzine-but weak is a relative term when you’re stacking it atop SSRI-induced synaptic serotonin saturation. One must ask: is the JAMA study truly representative, or merely a reflection of institutional inertia? The real danger lies not in the drug, but in the epistemic arrogance of clinicians who mistake statistical rarity for clinical insignificance. One patient’s rhabdomyolysis is not a footnote-it’s a symphony of systemic failure.
Paul Santos
10 December, 2025 . 19:05 PM
Fascinating how we’ve anthropomorphized serotonin into this mystical mood-god 🙏 while ignoring the fact that it’s just a neurotransmitter with a half-life of 20 minutes. Linezolid’s MAO-A inhibition? A minor blip in the grand cascade of neurochemical homeostasis. The real issue? We’re medicating normal human variation into pathology and then panicking when two pharmacological tools intersect. It’s not the drugs-it’s the narrative. 🤷♂️
Eddy Kimani
10 December, 2025 . 23:28 PM
This is actually a really nuanced discussion. I’m an ICU pharmacist and we’ve had 3 cases of suspected serotonin syndrome with linezolid in the last 5 years-all involved polypharmacy: SSRI + tramadol + dextromethorphan + high-dose linezolid. The single-agent cases? Almost nonexistent. The real takeaway: it’s not the combo of linezolid + one SSRI-it’s the polypharmacy soup. We now have a checklist in our EMR that flags all serotonergic agents when linezolid is ordered. It’s cut our false positives by 80%. Knowledge is power, but context is everything.
Chelsea Moore
12 December, 2025 . 18:35 PM
I can’t BELIEVE they’re downplaying this!! My cousin’s neighbor’s dog walker’s brother died from this!! It was on the news!! They said he was just taking Zoloft and then got linezolid and POOF-gone!! And now they’re saying it’s SAFE?? I’m telling everyone I know: DON’T TOUCH IT!! I’m not letting my mom near it!! This is a COVER-UP!!
John Biesecker
13 December, 2025 . 10:51 AM
you know what’s wild? we treat antibiotics like they’re magic bullets but forget they’re chemicals that interact with our bodies like a symphony. linezolid’s not evil-it’s just a tool that got repurposed. the real question is: why do we keep treating mental health meds like they’re fragile? serotonin isn’t a balloon you pop-it’s a river. sometimes you add a pebble, sometimes a log. it’s not the pebble-it’s the dam. maybe we need to stop fearing the combo and start asking: who’s managing the flow? 🌊🧠
Genesis Rubi
14 December, 2025 . 14:44 PM
USA rules. We don’t need some fancy JAMA study to tell us what’s safe. If your doc says linezolid, you take it. If you’re on antidepressants? You’re probably already weak anyway. Just don’t complain when your brain feels weird. We got better things to do than baby people.