Every year, people get the wrong medicine-not because of a mistake in diagnosis, but because two drugs look or sound too much alike. This isn’t rare. It’s one of the most common causes of preventable harm in hospitals and pharmacies. In the U.S., about one in four medication errors happens because a drug name was confused with another. That’s not a glitch. It’s a systemic problem built into how drugs are named, packaged, and spoken aloud.
What Exactly Are Look-Alike, Sound-Alike (LASA) Drugs?
Look-alike, sound-alike (LASA) drugs are medications that are easily mixed up because of their names, packaging, or appearance. This isn’t about typos or bad handwriting. It’s about names like HYDROmorphone and hYDROcodone. The difference? One letter is capitalized. But in a fast-paced hospital shift, when someone hears "hydro" and sees a vial labeled in all caps, the mistake can happen before anyone notices. There are three main ways these errors happen:- Orthographic (look-alike): The names look similar on paper or screen-like simvastatin 10 mg and simvastatin 20 mg. Even the same drug with different strengths can trip people up.
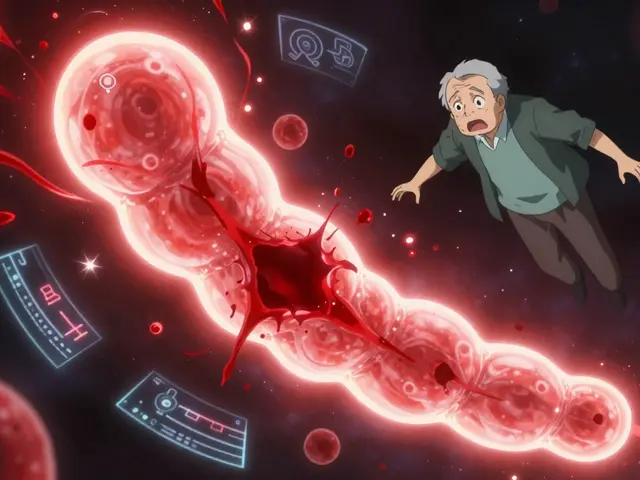
- Phonetic (sound-alike): The names sound the same when spoken-like vecuronium and versed. In a noisy ICU, a nurse might hear "versed" when the doctor said "vecuronium." One calms anxiety. The other paralyzes muscles. Mixing them can be fatal.
- Packaging or physical appearance: Two drugs come in nearly identical bottles, with similar colors, fonts, or label layouts. A pharmacist grabbing a vial during a rush might pull the wrong one without realizing it.
The Most Dangerous LASA Pairs
Some drug pairs are so dangerous they’re listed as high-alert by the Institute for Safe Medication Practices (ISMP). These aren’t just inconveniences-they’re potential killers.- Doxorubicin and daunorubicin: Both are chemotherapy drugs used for cancer. Confusing them can lead to severe organ damage or death.
- Insulin glargine and insulin lispro: One is long-acting, meant to last all day. The other is fast-acting, meant to be taken with meals. Giving the wrong one can send a diabetic patient into a coma.
- Clonidine and clonazepam: One lowers blood pressure. The other treats seizures and anxiety. Mix them up, and a patient could crash their blood pressure or have a seizure.
- Melphalan and meloxicam: Added to the high-alert list in 2024. One is a cancer drug. The other is a painkiller. A simple mix-up can lead to bone marrow failure.
- Naltrexone and naloxone: Both treat opioid overdose, but they work differently. Giving the wrong one can delay life-saving treatment.
Even small differences matter. A 2022 study found that simvastatin 10 mg and simvastatin 20 mg were the most frequently confused pair-because the strength is the only thing different on the label. In a busy pharmacy, that’s enough.
Why Do These Errors Keep Happening?
You’d think after decades of warnings, hospitals would have fixed this. But they haven’t. Why?- Drug names aren’t tested enough. The FDA approves new drug names based on limited review. Between 2018 and 2022, they rejected 34 new drug names just because they were too similar to existing ones. That’s progress-but it’s still not mandatory testing. Many names slip through.
- People are rushed. Nurses and pharmacists work under extreme pressure. During shift changes, night shifts, or when understaffed, even the most careful professionals miss details. One nurse on Reddit shared she almost gave levoTHYroxine instead of SYNTHROID because both vials looked identical and the doctor just said "thyroid med."
- Technology isn’t always used right. Electronic health records have alerts for LASA drugs, but many hospitals don’t turn them on, or they turn on too many alerts, causing "alert fatigue." Staff start ignoring them.
- Training is inconsistent. Some hospitals require annual LASA training. Others don’t. Oncology units, where dozens of similar chemotherapy drugs are used daily, often get extra training. General wards? Not so much.

What’s Being Done to Stop These Errors?
There are solutions-but they’re not perfect, and they’re not everywhere.- Tall Man Lettering: This is when part of a drug name is capitalized to highlight the difference-like HYDROmorphone vs. hYDROcodone. The FDA has applied this to over 200 drug pairs. But studies show it only works if staff actually notice and understand it. Some call it a "quasi-placebo effect." It helps-but it’s not a fix.
- Electronic alerts: Systems like Epic’s SafeMed have cut LASA errors by nearly 30% in some hospitals. But these tools only work if they’re properly configured and not buried under hundreds of other alerts.
- Standardized packaging: Some countries are moving toward color-coding, different bottle shapes, or unique label designs. Australia and the UK have made progress. The U.S. lags behind.
- AI voice recognition: A Johns Hopkins study funded by AHRQ is testing AI that listens to verbal medication orders and flags potential LASA confusions in real time. Early results show 89% accuracy. This could be a game-changer-if it gets adopted.
What You Can Do
If you’re a patient or caregiver, don’t assume the system will catch the mistake. Be your own safety net.- Ask: "What is this medication for?" and "How is it different from others I take?" If you’re on multiple pills, ask if any sound or look like each other.
- Check the label: Compare the name and strength on the bottle to what your doctor told you. Don’t rely on the pharmacist’s word alone.
- Speak up: If something feels off-like a pill that looks different than last time-ask. You’re not being difficult. You’re preventing harm.
- Know your high-risk drugs: If you take insulin, anticoagulants like warfarin, opioids, or chemotherapy drugs, learn the exact names and strengths. Keep a written list.
The Bigger Picture
This isn’t just about a few bad names. It’s about how we design systems. We’ve accepted that humans will make mistakes. But we don’t have to design systems that make those mistakes easy.The World Health Organization says we need to stop blaming individuals and start fixing the system. That means:
- Requiring strong, standardized testing for all new drug names before approval
- Creating global rules for packaging and labeling
- Investing in AI and technology that works for real-world conditions-not just in labs
- Ensuring every hospital, no matter how small, has a tailored LASA list and training
Right now, only 72% of large U.S. hospitals have full LASA protocols. In smaller clinics and rural pharmacies? It’s under 40%. That’s not just a gap. It’s a danger zone.
There’s hope. The global market for medication safety tech is growing fast-projected to hit $6.8 billion by 2027. But money alone won’t fix this. We need policy, training, and culture change. And we need it now.
Frequently Asked Questions
What are the most common LASA drug pairs?
The most common pairs include HYDROmorphone and hYDROcodone, insulin glargine and insulin lispro, clonidine and clonazepam, doxorubicin and daunorubicin, and simvastatin 10 mg versus simvastatin 20 mg. In 2024, ISMP added melphalan/meloxicam and naltrexone/naloxone to their high-alert list.
How many people die from LASA errors each year?
Between 2018 and 2022, the FDA’s MAUDE database recorded at least 128 deaths directly linked to look-alike, sound-alike medication errors. Experts believe the real number is higher, as many cases go unreported or misclassified.
Is Tall Man Lettering enough to prevent errors?
No. While Tall Man Lettering (like HYDROmorphone) helps highlight differences, studies show it only works if staff are trained to notice it. Many don’t. It’s a helpful tool, but not a solution on its own. It should be used alongside electronic alerts, training, and packaging changes.
Can I trust my pharmacist to catch these errors?
Pharmacists are trained to catch errors-but they’re often overwhelmed. During busy hours, especially at night or during shift changes, even experienced staff can miss subtle differences. Always double-check your medication name, strength, and purpose before taking it.
What should I do if I think I received the wrong medication?
Stop taking it. Call your pharmacist or doctor immediately. Don’t wait to see if you feel different. If you’re unsure, take the bottle to a different pharmacy for a second check. Your safety is more important than avoiding an awkward conversation.
Are there any new technologies helping reduce these errors?
Yes. AI-powered voice recognition systems are being tested to catch LASA errors during verbal orders. Epic’s SafeMed module has reduced errors by 28.7% in pilot hospitals. Some countries are also testing unique bottle shapes and color-coded labels to make visual confusion harder. These tools are promising-but they’re not yet standard everywhere.
Next Steps
If you’re a patient: Make a list of all your medications. Write down the exact name and strength. Keep it with you. Ask your doctor or pharmacist: "Are any of these drugs easy to mix up?" If you’re a healthcare worker: Review your facility’s LASA list. If you don’t have one, ask for it. Push for training. Use Tall Man Lettering in your notes. Speak up when you see a risky pairing.Medication safety isn’t just about rules. It’s about awareness. And awareness starts with knowing these names aren’t accidents-they’re preventable risks.





Chris Park
6 December, 2025 . 22:44 PM
Let’s be real-this isn’t about drug names. It’s about the FDA being a corrupt oligopoly that lets pharma giants name drugs like they’re marketing cereal. HYDROmorphone vs hYDROcodone? That’s not an accident. That’s a feature. They want you to mess up so you need more prescriptions to fix the side effects. The capitalization trick? A placebo for the gullible. Real safety would mean banning all generic names and forcing each drug to have a unique, nonsensical alphanumeric code. Like XQ-9927B. No one could confuse that. But then Big Pharma wouldn’t own the brand recognition. So we get chaos. And profit.
Inna Borovik
8 December, 2025 . 21:01 PM
Interesting breakdown, but you’re missing the real elephant in the room: liability avoidance. Hospitals don’t fix LASA errors because if you prevent a mistake, you don’t get the lawsuit payout. The system is designed to absorb blame at the nurse level, not the corporate one. That’s why training is inconsistent-it’s cheaper to let someone die than to overhaul 12,000 pharmacy systems. And don’t get me started on how insurance companies refuse to cover AI voice recognition because it cuts their ‘human error’ reimbursement loopholes.
Jackie Petersen
9 December, 2025 . 08:50 AM
Ugh. Another ‘let’s blame the system’ post. Meanwhile, I’ve been working in a rural pharmacy for 18 years and I’ve never once mixed up insulin glargine and lispro. It’s not the system-it’s the lazy, distracted millennials who can’t read a label. We used to have to memorize drug names. Now? They just tap a screen and trust the computer. And when it fails, they cry about ‘systemic issues.’ Fix your own eyesight first.
Annie Gardiner
9 December, 2025 . 21:35 PM
What if the problem isn’t the drugs… but our obsession with control? We think we can name things perfectly and expect the world to obey. But life is messy. Maybe we should stop trying to engineer away human error and just accept that people will make mistakes. Maybe the real solution is to stop giving so many damn drugs in the first place. I mean… do we really need 17 different painkillers that all sound like they’re from a sci-fi movie? Maybe the answer isn’t taller letters… but fewer letters.
joanne humphreys
11 December, 2025 . 00:43 AM
I’ve been a nurse for 22 years and I’ve seen this play out too many times. The Tall Man Lettering helps-but only if you’re not exhausted. I once pulled clonidine instead of clonazepam at 3 a.m. after a 14-hour shift. I caught it because I paused and said the name out loud. That’s it. No tech. No AI. Just me, tired, and a second of silence. We need more pauses in the system, not more alerts. People aren’t machines. We need space to breathe before we push ‘administer.’
Kumar Shubhranshu
12 December, 2025 . 05:22 AM
Insulin glargine and lispro are the worst. I saw a patient go into coma because nurse picked wrong bottle. No excuse. Pharmacist should have double checked. Everyone is too busy. Everyone thinks someone else will catch it. Bad system. But also bad people. Stop blaming tech. Train better. Check twice. Simple.
Mayur Panchamia
12 December, 2025 . 13:47 PM
Oh, so now it’s ‘systemic’? Let me guess-the FDA is owned by Big Pharma, and the WHO is a tool of globalists trying to control our medicine! We don’t need AI voice recognition-we need to ban foreign drug names! Why are we letting Chinese and Indian labs name our pills? ‘Melphalan’? Sounds like a space virus! ‘Naltrexone’? That’s not even English! We need American-sounding names-like ‘AmericanHeal-12’ or ‘PatriotPill-X’-so no one gets confused. And if you can’t read it? That’s your problem, not ours!
Karen Mitchell
12 December, 2025 . 20:27 PM
While the intent of this article is laudable, the underlying assumption-that human error is a systemic failure rather than a moral one-is deeply flawed. The solution is not technological augmentation, but the cultivation of professional virtue. Nurses and pharmacists are entrusted with life-and-death responsibilities. If they cannot distinguish between two similarly named medications, they are unfit for the role. No algorithm will compensate for a lack of diligence. The real crisis is not in nomenclature, but in the erosion of professional standards.
Kenny Pakade
13 December, 2025 . 01:24 AM
AI voice recognition? That’s the dumbest thing I’ve heard since ‘smart’ refrigerators. Who’s gonna pay for that? Taxpayers? No. The only thing that works is discipline. I worked in a VA hospital. We had a rule: if a drug name had ‘-ine’ or ‘-one’ in it, you had to say it out loud and spell it to the patient. No exceptions. No alerts. No tech. Just human accountability. And guess what? We had zero LASA errors for five years. You don’t need fancy gadgets. You need people who care enough to slow down. But hey, let’s just throw money at a robot and call it progress.
brenda olvera
13 December, 2025 . 16:29 PM
I’m from Mexico and we don’t have fancy AI or tall man letters but we have something better-community. My abuela always asked the pharmacist: ‘¿Es esta la que me da energía o la que me calma?’ She didn’t know the names, but she knew what they did. We need to teach patients to ask simple questions. Not just ‘what is this?’ but ‘what does this do to me?’ That’s real safety. Not tech. Not labels. Just connection. And maybe, just maybe, we’ll stop treating people like inventory.