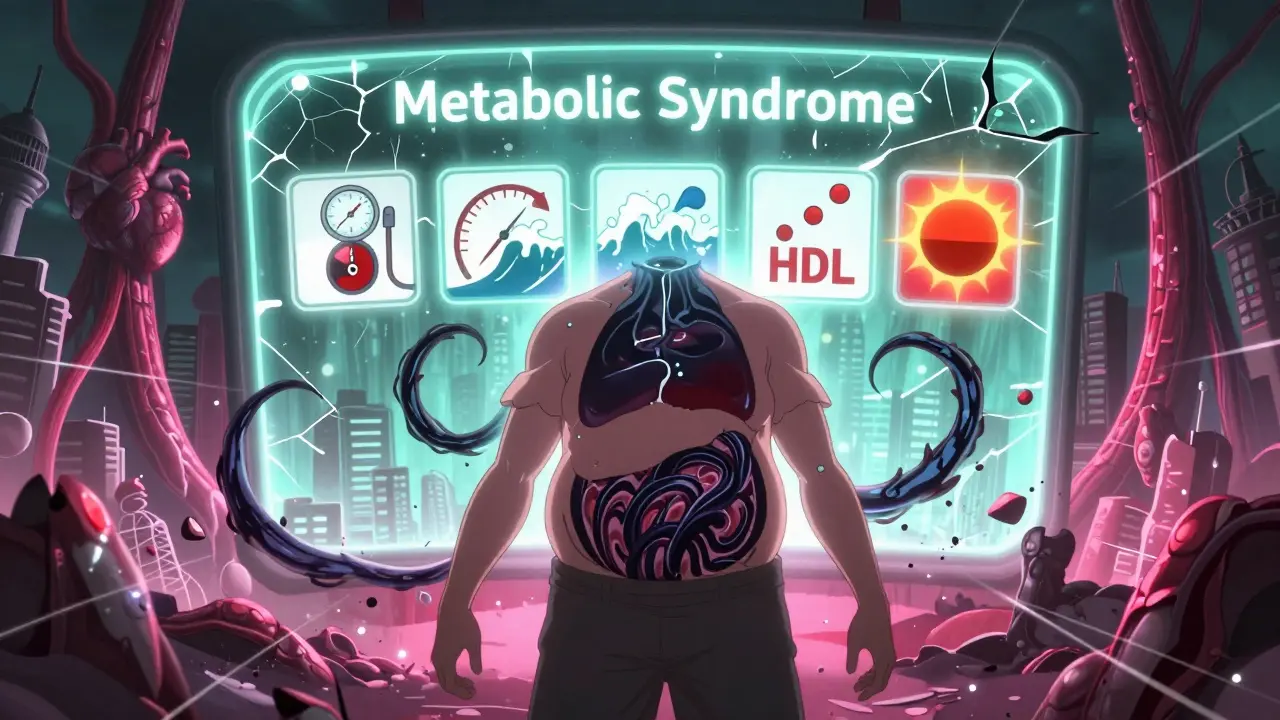
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one disease-it’s a group of warning signs that show your body is struggling to manage energy. If you have three or more of these, you’re diagnosed with it: too much fat around your waist, high blood pressure, high triglycerides, low HDL (the "good" cholesterol), and high fasting blood sugar. These don’t happen by accident. They’re linked. And together, they push your risk for heart disease, stroke, and type 2 diabetes way up.
Think of it like a slow leak in your car’s engine. Individually, each issue-low oil, overheating, bad fuel-might not stop you. But together? You’re headed for a breakdown. That’s metabolic syndrome. It’s silent. You won’t feel it until something serious happens. The only obvious clue? A growing waistline. An "apple shape," where fat piles up around your middle, not your hips.
Abdominal Obesity: More Than Just Extra Weight
Not all fat is the same. Fat under your skin (subcutaneous) is mostly harmless. But fat inside your belly, wrapped around your liver and organs (visceral fat), is dangerous. This is the kind that drives metabolic syndrome.
Doctors measure it with a tape measure. For men, a waist over 102 cm (40 inches) raises red flags. For women, it’s 88 cm (35 inches). These numbers drop even lower for people of Asian descent-90 cm for men, 80 cm for women-because their bodies are more sensitive to visceral fat.
Why does it matter? Visceral fat isn’t just storage. It’s active. It releases fatty acids straight into your liver, which scrambles your blood sugar and cholesterol. It also pumps out inflammatory chemicals. That’s why someone with a big belly but normal weight elsewhere can still have metabolic syndrome. It’s not about the scale-it’s about where the fat lives.
High Blood Pressure: The Quiet Threat
High blood pressure doesn’t come with symptoms. No headaches, no dizziness. That’s why it’s called the "silent killer." But in metabolic syndrome, it’s one of the big three. A reading of 130/85 mmHg or higher counts-even if you’re on medication to control it.
This isn’t just about stress or salt. It’s tied to insulin resistance. When your cells stop responding well to insulin, your kidneys hold onto more sodium and water. Your blood vessels tighten. Your heart works harder. Over time, that damages arteries, increases plaque buildup, and raises stroke risk.
What’s surprising? Many people with metabolic syndrome have high blood pressure without knowing it. Routine checkups are the only way to catch it. And if you’re over 40, or carry extra weight around your middle, you should be checking it at least once a year.
Lipid Problems: Triglycerides Up, HDL Down
Your blood fats tell a story. High triglycerides and low HDL cholesterol are classic signs of metabolic syndrome.
Triglycerides above 150 mg/dL mean your body is converting too many carbs and sugars into fat. This often happens when you eat too much refined food, drink sugary drinks, or don’t move enough. Your liver gets overloaded and starts storing fat instead of burning it.
Meanwhile, HDL-the "good" cholesterol that clears out bad fats from your arteries-plummets. For men, it drops below 40 mg/dL. For women, below 50 mg/dL. That’s not random. Insulin resistance directly lowers HDL production. So you end up with more gunk in your blood and less cleanup crew to remove it.
These two lipid changes together are like a one-two punch: more plaque-forming particles, fewer protectors. That’s why people with metabolic syndrome often end up on statins-not just for cholesterol, but to reduce inflammation and stabilize artery walls.

Why Insulin Resistance Is the Core Problem
At the heart of metabolic syndrome is insulin resistance. It’s not diabetes yet-but it’s the road that leads there.
Insulin is your body’s key to unlock cells and let glucose in for energy. When you eat too much sugar and refined carbs over years, your cells start ignoring insulin. Your pancreas responds by pumping out more insulin to compensate. That’s called hyperinsulinemia.
But high insulin levels do more than just raise blood sugar. They tell your liver to make more fat. They make your kidneys hold onto salt, raising blood pressure. They suppress the enzyme that breaks down triglycerides, so they pile up. And they lower HDL. It’s all connected.
Studies show insulin resistance can start decades before diabetes shows up. That’s why catching metabolic syndrome early is so powerful. You’re not just treating numbers-you’re stopping a chain reaction before it breaks your heart or pancreas.
Who’s at Risk? It’s Not Just About Age
One in three American adults has metabolic syndrome. In the UK, numbers are similar. But it’s not evenly spread.
Age matters. Around 20% of people in their 20s have it. By 60, it’s nearly 50%. But it’s also hitting younger people harder than ever. Kids with obesity are now showing early signs. Why? Processed foods, sugary drinks, sitting all day.
Genetics play a role too. If your parents had diabetes or heart disease, you’re more likely to develop metabolic syndrome. Ethnicity counts: African Americans, Hispanics, Native Americans, and South Asians have higher rates-even at lower body weights.
Women with polycystic ovary syndrome (PCOS) are at especially high risk. Their insulin resistance is often more severe. And if you’ve had gestational diabetes, your chance of developing metabolic syndrome later jumps dramatically.
Can You Reverse It? Yes-But It Takes Work
Here’s the good news: metabolic syndrome is reversible. Not with pills. With lifestyle.
Research shows losing just 5-10% of your body weight can slash triglycerides, lower blood pressure, improve insulin sensitivity, and raise HDL. That’s not about extreme diets. It’s about consistency.
Start with movement. At least 150 minutes a week of brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. You don’t need a gym. Just move more. Walk after meals. Take stairs. Park farther away.
Diet changes are even more critical. Cut out sugary drinks, white bread, pastries, and fried foods. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats like olive oil and avocado. Fiber is your friend-it slows sugar absorption and helps your gut bacteria stay balanced.
One program at Penn Medicine reversed metabolic syndrome in 65% of patients over 12 months using this approach. Not drugs. Not surgery. Just food, movement, and support.

When Medication Becomes Necessary
Lifestyle is first. Always. But sometimes, you need help.
If your blood pressure stays high despite diet and exercise, your doctor may prescribe an ACE inhibitor or calcium channel blocker. If triglycerides are sky-high or HDL stays stubbornly low, statins or fibrates might be added. For blood sugar, metformin is often used-not to treat diabetes, but to improve insulin sensitivity and prevent it.
But here’s the catch: meds don’t fix the root. They manage symptoms. If you stop eating well and moving, the numbers will creep back up. Medication buys time-but lifestyle rebuilds your metabolism.
What Happens If You Ignore It?
Ignoring metabolic syndrome is like ignoring a warning light on your dashboard. The car might still run-for a while.
But over time, the damage adds up. Your arteries harden. Your heart muscle thickens. Your pancreas burns out. Your kidneys struggle. Your risk of heart attack doubles. Your chance of getting type 2 diabetes goes up fivefold.
Studies tracking people for over a decade show that those with metabolic syndrome are far more likely to die from heart disease than those without it. Even if you don’t get diabetes, your cardiovascular risk stays high.
The longer you wait, the harder it gets to reverse. Early action is the only real advantage you have.
What Should You Do Next?
Start with your doctor. Ask for a full metabolic panel: waist measurement, blood pressure, fasting glucose, triglycerides, HDL. Don’t wait for symptoms. If you’re over 40, overweight, or have a family history of diabetes or heart disease, get checked now.
Write down your numbers. Track them. Set small goals: lose 5 pounds. Walk 20 minutes after dinner. Swap soda for sparkling water. Celebrate progress, not perfection.
Metabolic syndrome isn’t your fault. But fixing it? That’s your power. You don’t need to be perfect. You just need to be consistent.
Can you have metabolic syndrome without being overweight?
Yes, but it’s rare. Most people with metabolic syndrome carry excess weight, especially around the belly. However, some people with normal BMI can still have high visceral fat due to genetics, inactivity, or poor diet. This is sometimes called "TOFI"-thin on the outside, fat inside. Waist measurement is more telling than weight alone.
Does metabolic syndrome always lead to diabetes?
No, but it greatly increases the risk. About 5 out of 10 people with metabolic syndrome will develop type 2 diabetes within 10 years if nothing changes. The good news? Losing 5-7% of body weight and getting 150 minutes of exercise a week can cut that risk by more than half.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one possible component, but it also requires at least two other factors: high blood pressure, bad cholesterol, or abdominal obesity. You can have prediabetes without metabolic syndrome-and vice versa.
Can children get metabolic syndrome?
Yes, and it’s rising fast. With childhood obesity rates climbing, kids as young as 10 are showing signs: high waist circumference, elevated blood pressure, and abnormal cholesterol. Early intervention with diet, activity, and sleep habits can prevent lifelong health problems.
Do I need to take medication for life if I’m diagnosed?
Not if you change your lifestyle. Many people who lose weight, eat better, and move more can reduce or even stop their medications under medical supervision. But if you return to old habits, the conditions will come back. Medication is a tool, not a cure.
Final Thought: It’s Not a Life Sentence
Metabolic syndrome sounds scary. But it’s not a death sentence. It’s a signal. A chance to reset. You don’t need to overhaul your life overnight. Just start. One healthier meal. One extra walk. One less sugary drink. Small steps, repeated daily, rebuild your metabolism. And that’s how you take back your health.