State Pharmacy Laws: What You Need to Know About Prescription Rules and Patient Rights
When you walk into a pharmacy, you might think it’s just about getting your pills. But behind the counter, state pharmacy laws, rules set by individual U.S. states that govern how medications are dispensed, who can prescribe them, and how pharmacies operate. Also known as pharmacy regulations, these laws shape everything from whether you can get a generic instead of a brand drug, to whether your insurance can force a switch without your doctor’s approval. These aren’t federal rules—they change from New York to Texas, and they directly impact your access, cost, and safety.
One major area where state pharmacy laws show up is in generic drug rules, policies that determine when pharmacists can substitute brand-name drugs with cheaper generics, and when they must get your doctor’s permission first. Some states require explicit consent before switching, others let pharmacists swap automatically unless you say no. That’s why you might get a different pill than what your doctor wrote—and why you need to know your rights. These rules connect to pharmacy reimbursement, how pharmacies get paid for each prescription, often through complex formulas set by PBMs and state Medicaid programs. When reimbursement rates drop too low, pharmacies struggle to stay open, especially in rural areas. That’s not just a business problem—it’s a healthcare access issue.
Then there’s patient rights, legal protections that stop insurers from slapping you with surprise bills, forcing you into financing plans, or combining consent forms for unrelated treatments. New York’s 2024 laws, for example, banned combined consent forms and made it illegal to use medical debt to hurt your credit. Other states are following suit. These protections don’t come from federal law alone—they’re often pushed through state legislatures because patients spoke up. And if you’ve ever been told you can’t get your brand medication because of insurance rules, that’s a direct result of how state laws interpret the No Surprises Act and other federal policies.
These laws also affect how drugs are tracked. If you’re on a biosimilar or a psychiatric combo med, state laws determine whether pharmacies must record the exact product you got—and whether that info is shared with your doctor. That matters because small differences in generic versions can change how your body responds. And if you lose your meds while traveling, state laws control whether a pharmacist can refill an out-of-state prescription without a new doctor’s note.
What you’ll find below are real stories and guides from people who’ve fought these systems—whether it’s pushing back on a generic switch, dealing with a drug interaction caused by state-level formulary rules, or navigating reimbursement chaos that left pharmacies unable to stock their meds. These aren’t abstract policies. They’re daily hurdles. And understanding them gives you power.
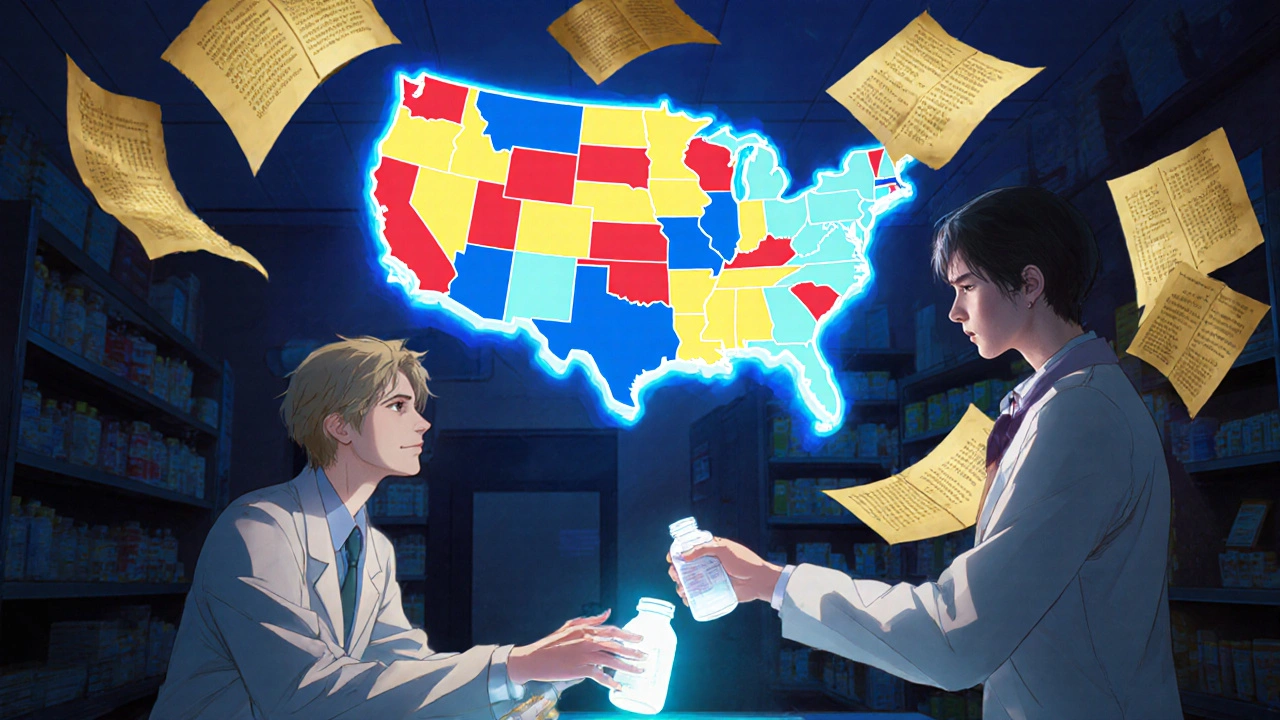
How Generic Substitution Laws Work: State-by-State Breakdown
Generic substitution laws vary widely across U.S. states, affecting how and when pharmacists can swap brand-name drugs for cheaper generics. Learn how each state regulates substitutions, who must give consent, and why some drugs are exempt.
View More