Managing medications at home can be overwhelming-especially for older adults taking five, ten, or even more pills a day. Missed doses, wrong times, confusing instructions, or dangerous drug interactions aren’t just inconveniences-they can land someone in the hospital. That’s where home health services for medication management come in. These aren’t just helpers dropping off pills. They’re trained professionals who organize, monitor, and support safe medication use right in your home.
What Home Health Medication Management Actually Does
Home health services for medication management go beyond reminding someone to take their pills. They create a full safety system around medications. A nurse or certified medication aide will start by making a complete, up-to-date list of every drug the patient is taking-including prescriptions, over-the-counter meds, vitamins, and supplements. This list includes the name (brand and generic), dose, time of day, why it’s prescribed, and any known side effects or warnings.This list doesn’t stay on a piece of paper. It’s shared with every doctor, pharmacist, and specialist involved in the patient’s care. Why? Because one doctor might prescribe a blood thinner, and another might prescribe an anti-inflammatory-without knowing the other is doing it. That’s how dangerous interactions happen. According to MedPro’s 2022 analysis, medication errors cause about 30% of adverse events in home care. Proper medication reconciliation cuts that risk by 60%.
Home health workers also check for duplicates. One patient might be taking both a generic and brand-name version of the same drug, or two different pills with the same active ingredient. Phoenix Home Care’s case studies found their staff caught 12 potential drug interactions in just six months across 200 patients-just by reviewing the list.
Tools That Make a Real Difference
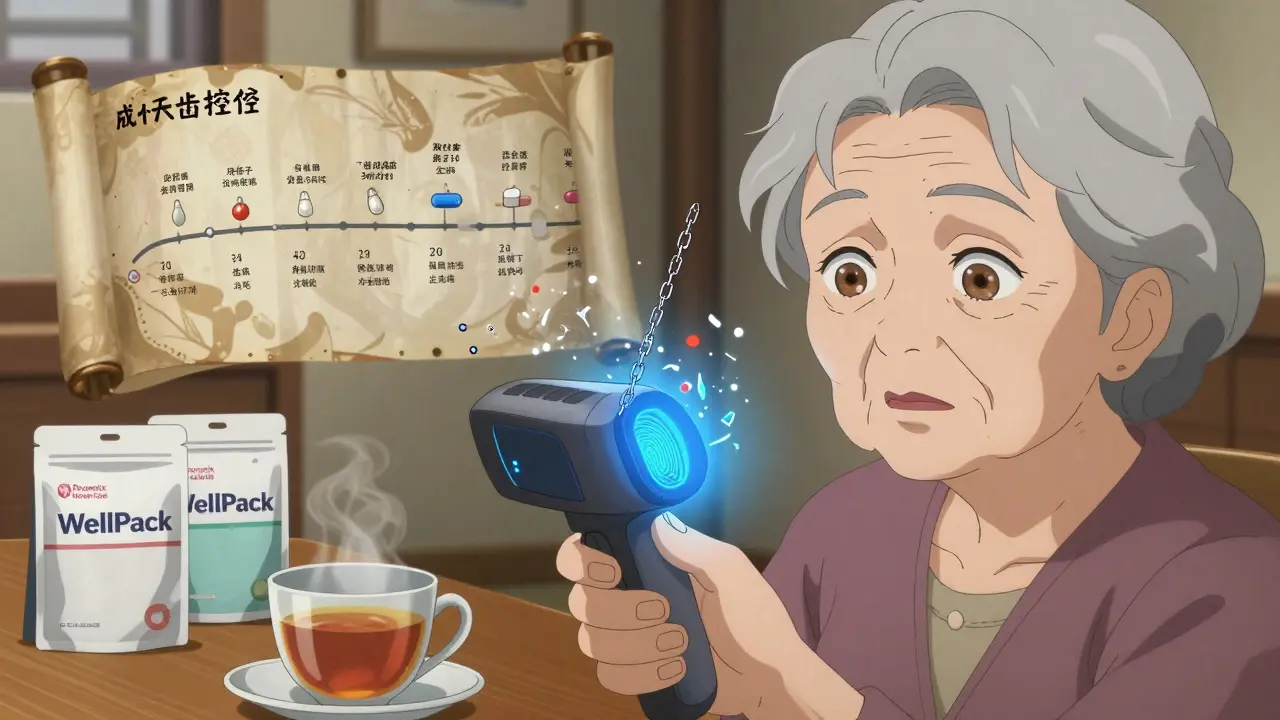
Organizing pills is one of the biggest challenges. A pillbox might seem simple, but the right one can cut missed doses by 45%. The most effective systems use daily or weekly compartments labeled with times like “Morning,” “Afternoon,” “Evening,” and “Bedtime.” Some go further-like Phoenix Home Care’s WellPack system, which puts each day’s pills into sealed, labeled pouches. No sorting needed. Just open and take.Digital tools help too. Smartphone apps with alarms and reminders boost adherence by 35%. But not everyone is comfortable with tech. That’s why many home health agencies now use visual aids: large-print charts with simple icons, color-coded by time of day, and printed in the patient’s preferred language. A Clarest survey found 67% of caregivers said these visuals made a huge difference in understanding.
Some newer systems even use biometric verification. CritiCare’s 2023 app requires a fingerprint or facial scan before a dose is marked as taken. This prevents someone else from taking the pill-or the patient from forgetting they already took it. In pilot programs, this reduced errors by 40%.
Who Qualifies for These Services?
Medicare Part A covers home health medication management-but only under strict conditions. You must be homebound, need skilled nursing or therapy, and have a doctor certify that you need these services. It’s not for daily reminders if you’re otherwise independent. If you’re recovering from a hospital stay, have a new diagnosis like heart failure or diabetes, or just had surgery, you’re likely eligible.But what if you need help every day? Medicare won’t cover that. That’s where private home care agencies come in. Companies like Clarest and Phoenix Home Care offer daily medication management for $20-$40 per hour. It’s not cheap, but consider this: a single preventable hospital readmission costs an average of $1,200 per month in avoidable expenses. Professional help pays for itself.
Medicare Advantage plans are starting to cover more. Some now include continuous monitoring devices that track when pills are taken and alert family or nurses if a dose is missed. These are still new, but expect wider coverage by 2025.
How It Works: A Step-by-Step Process
Getting started isn’t complicated. Here’s what typically happens:- Assessment: A nurse visits your home to review all medications, talk to you and your family, and check your living space for safety risks.
- Reconciliation: They compare your current list with hospital records and pharmacy logs to spot duplicates, missing meds, or outdated prescriptions.
- Planning: A schedule is created using pill organizers, apps, or visual charts. They’ll align doses with your daily routine-like taking blood pressure meds after breakfast.
- Training: You or your caregiver learns how to use the system. The “teach-back” method is used: you explain it back to them to make sure you got it right.
- Monitoring: Staff visit regularly-weekly, biweekly, or daily-to check adherence, update the list, and report changes to your doctor.
For simple regimens (1-3 meds), it usually takes 2-3 visits. For complex ones (8+ meds), it can take 6-8 sessions. The goal isn’t just to get you started-it’s to make sure the system keeps working long-term.
What to Watch Out For
Even with professional help, problems can happen. One of the biggest issues is communication gaps. John T. from Reddit shared how inconsistent handoffs between agencies led to a dangerous interaction between blood thinners that sent him to the ER. That’s why it’s critical that your home health agency coordinates directly with your doctor and pharmacy.Another issue: timing. Some meds need to be taken exactly at 7 a.m. and 7 p.m. But what if your caregiver can’t come at 7 a.m.? That’s why flexible systems matter. Some agencies now offer “on-demand” visits or use smart pill dispensers that lock and unlock at scheduled times.
Also, don’t assume all agencies are the same. Only 65% of home health agencies consistently do full medication reconciliation during care transitions, even though CMS requires it. Ask: “Do you use a standardized checklist? Do you update the list within 24 hours of any change?” If they hesitate, look elsewhere.

Real Results People See
Mary K. from Ohio used Phoenix Home Care’s WellPack system for her mother with dementia. Before, her mother missed 30% of her doses. Within two weeks, that dropped to under 5%. “It was like a miracle,” she said. “I stopped worrying every morning.”Clarest’s 2023 survey of 500 caregivers showed 78% saw better adherence with professional help. And the numbers back it up: patients using home health medication management have a 20% lower chance of being readmitted to the hospital within 30 days.
It’s not just about safety-it’s about peace of mind. For families, knowing someone trained is checking the meds, watching for side effects, and calling the doctor when something’s off? That’s priceless.
What’s Next for Home Health Medication Services
The field is changing fast. By 2025, 65% of agencies are expected to use AI tools that scan for drug interactions in real time. Imagine a system that flags a new prescription against your entire list before it’s even filled. That’s coming.Language support is expanding too. Phoenix Home Care now includes QR codes on pill pouches that link to instructional videos in 17 languages. For non-English speakers, this removes a major barrier.
But there’s a big risk: staffing. The National Association for Home Care & Hospice reports a 28% vacancy rate for home health nurses in 2023. That means longer wait times and overworked staff. If you’re choosing a provider, ask about their turnover rate and training standards.
For now, the best path is clear: if you or a loved one is managing multiple medications at home, professional support isn’t a luxury-it’s a necessity. The tools exist. The data proves it works. The question isn’t whether you can afford it. It’s whether you can afford not to.
Can home health services help if someone has dementia or memory problems?
Yes. Home health services are especially helpful for people with dementia or memory loss. Staff use visual aids, sealed daily pouches, and digital reminders that can’t be ignored. They also monitor for signs of confusion or side effects. Many families report that their loved ones become more consistent with meds and less anxious when they know someone is helping them take them correctly.
Does Medicare pay for daily medication management?
Medicare Part A only covers intermittent skilled nursing visits-for example, a nurse coming twice a week to check meds after a hospital stay. It does not cover daily assistance unless you’re also receiving therapy or skilled care. For daily help, you’ll need private pay or a Medicare Advantage plan that includes extra benefits. Always check with your plan before signing up.
How do I know if my parent needs professional medication help?
Look for signs: missed doses, pills scattered around the house, empty pill bottles that shouldn’t be empty, or confusion about what each pill is for. If they’re taking five or more medications, or have recently been hospitalized, they’re at higher risk. A simple test: ask them to show you their pill schedule. If they can’t explain it clearly, it’s time to call a home health agency.
Can home health workers give injections or IV meds?
Yes, if they’re licensed nurses. Most home health agencies employ registered nurses who can administer injections, IV medications, and wound care. But this is different from basic pill management. You’ll need a doctor’s order and Medicare or insurance approval for these services. Always confirm what level of care the agency provides before hiring them.
What if my parent doesn’t want help with their meds?
Respect their autonomy, but don’t ignore the risk. Try framing it as “help” rather than “control.” Say, “I don’t want you to forget your heart pill,” instead of “You need someone to manage your meds.” Involve their doctor-they’re more likely to listen to a professional. Many agencies offer a free initial visit just to talk, with no pressure to sign up.
How often should the medication list be updated?
Every time there’s a change-new prescription, dose adjustment, or drug stopped. CMS requires documentation within 24 hours. A good agency will review the full list monthly and update it immediately after any doctor visit. Ask for a copy of the latest version after each visit. Keep it in a visible place, like on the fridge.
Are home health medication services available in rural areas?
Availability varies. Urban areas have more options, but many rural agencies have adapted with telehealth check-ins and mobile teams that cover wider regions. Medicare-certified agencies must serve all areas they’re licensed in. Call your local Area Agency on Aging-they can connect you with providers in your county, even if they’re a drive away.
Can I use home health services for my pet’s medications?
No. Home health services are designed for human patients under Medicare or private health regulations. Pet medications require veterinary care. Some veterinary home care services exist, but they’re separate and not covered by health insurance.