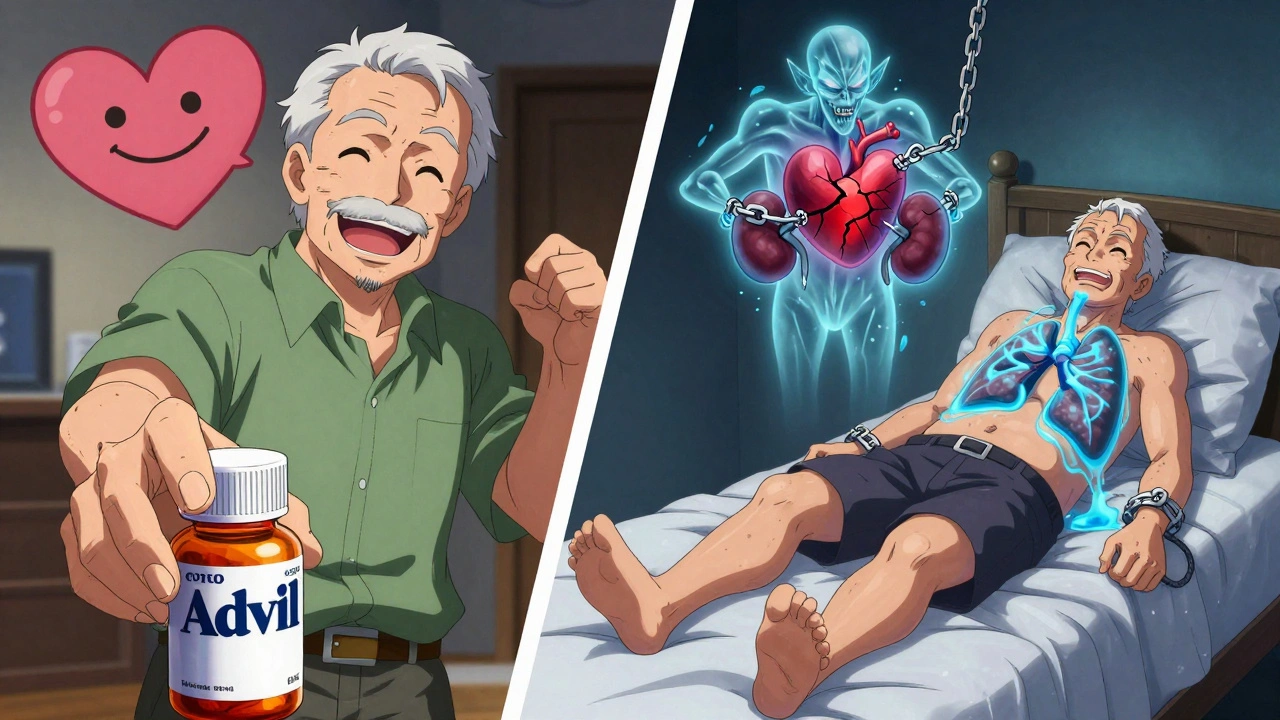
If you have heart failure, taking an over-the-counter painkiller like ibuprofen or naproxen might seem harmless-until your ankles swell, your weight jumps overnight, and you’re gasping for air. This isn’t rare. It’s a direct, well-documented consequence of NSAIDs interfering with how your heart and kidneys work together. And it can land you back in the hospital-sometimes within just a few days.
Why NSAIDs Are Dangerous for Heart Failure Patients
NSAIDs-non-steroidal anti-inflammatory drugs-work by blocking enzymes called COX-1 and COX-2. These enzymes help produce prostaglandins, chemicals that cause pain and inflammation. But prostaglandins also play a vital role in keeping your kidneys functioning properly, especially when your heart is weak.
In heart failure, your heart can’t pump blood effectively. Your body responds by activating systems that hold onto salt and water to maintain blood pressure. Normally, prostaglandins help balance this by encouraging your kidneys to flush out extra sodium. When you take an NSAID, you shut down that safety valve. Sodium builds up. Water follows. Your blood volume increases. Your heart, already struggling, now has to work harder. The result? Fluid backs up into your lungs, legs, and abdomen. That’s acute decompensated heart failure.
This isn’t theoretical. A 2022 study tracking over 100,000 people with type 2 diabetes in Denmark found that even a few days of NSAID use raised the risk of heart failure hospitalization by up to 88%. The highest risk? The first week. That’s faster than most people realize.
It’s Not Just Prescription NSAIDs
Many people think the danger only comes from strong, prescription-strength NSAIDs. It doesn’t. Over-the-counter pills like Advil, Aleve, and Motrin carry the same risks. In fact, because they’re easy to get, they’re more dangerous. A 2018 American Heart Association survey found that 37% of heart failure patients had taken NSAIDs without knowing they were risky. Of those, 62% ended up needing urgent medical care.
One Reddit user from Melbourne described how he took two 400mg ibuprofen tablets for a bad back after his doctor told him his heart failure was stable. Within 72 hours, he gained 4.5 kilograms (10 pounds) in fluid. He couldn’t walk to the bathroom without stopping to catch his breath. He ended up in the emergency room. His doctor said the NSAIDs had triggered his heart failure to flare up-fast.
Even so-called "safer" NSAIDs like celecoxib (Celebrex) aren’t safe for heart failure patients. Early hopes that COX-2 inhibitors would spare the kidneys turned out to be wrong. The same 2003 review by Bleumink and others showed that these drugs cause identical fluid retention. No NSAID is risk-free in heart failure.
Who’s Most at Risk?
The older you are, the higher your risk. Most heart failure patients are over 65. Their kidneys are already less efficient. Their bodies hold onto salt more easily. And they’re more likely to be taking multiple medications-some of which, like diuretics or ACE inhibitors, can be weakened by NSAIDs.
People with type 2 diabetes are especially vulnerable. Their kidneys are often already stressed. A 2022 study showed that even short-term NSAID use in this group led to hospitalizations at rates 1.8 times higher than normal. The same applies to those with high blood pressure or chronic kidney disease.
It’s not just about existing conditions. If your heart failure is newly diagnosed, or if you’ve recently been discharged from the hospital, your body is still unstable. NSAIDs can tip the balance. The 2024 Global Heart Failure Registry found that patients exposed to NSAIDs within 30 days of discharge had a 28% higher chance of being readmitted.
What Happens When You Take Them?
Symptoms don’t always appear slowly. Many patients notice changes within 24 to 72 hours:
- Sudden weight gain (1-2 kg or more in a few days)
- Swelling in the ankles, legs, or belly
- Shortness of breath, even at rest
- Feeling more tired than usual
- Need to sleep propped up because lying flat makes breathing hard
These aren’t "just side effects." They’re signs your heart is failing again-because of the NSAID. That’s why doctors tell patients to weigh themselves daily. A 2-kilogram (4.4-pound) weight gain in 24 hours is a red flag. It’s not fat. It’s fluid. And it’s dangerous.
What Can You Take Instead?
Acetaminophen (paracetamol, Tylenol) is the go-to alternative. It doesn’t affect kidney blood flow or sodium retention. It won’t reduce inflammation like NSAIDs do, but for most types of pain-headaches, muscle aches, arthritis discomfort-it works well enough.
For more severe pain, non-drug options matter. Physical therapy, heat packs, gentle stretching, and even acupuncture can help. If you have arthritis or joint pain, your doctor might suggest corticosteroid injections or disease-modifying drugs instead of daily NSAIDs.
And yes-your family can help. A 2024 MedlinePlus guide says caregivers should check medicine cabinets for NSAIDs, read labels on cold and flu remedies (many contain ibuprofen or naproxen), and ask pharmacists before buying anything new. Don’t assume "natural" or "herbal" pain relievers are safe either. Some, like willow bark, act like aspirin and carry the same risks.
What Doctors Are Doing About It
The European Society of Cardiology, the American College of Cardiology, and the American Heart Association all agree: NSAIDs are absolutely contraindicated in heart failure. That means they should not be used at all. The guidelines are clear. The evidence is overwhelming.
But prescribing habits haven’t caught up. A 2020 study found that over 15% of heart failure patients still got NSAID prescriptions within a year of diagnosis. In some cases, doctors didn’t realize the patient had heart failure. In others, they assumed the pain was worth the risk. A 2021 survey showed that only 43% of primary care doctors routinely ask heart failure patients about NSAID use during medication reviews.
Regulators have tried to fix this. The U.S. FDA updated NSAID labels in 2020 to warn of heart failure risk. The European Medicines Agency did the same in 2013-and reinforced it after the 2022 Danish study. But warnings on a pill bottle don’t always reach the right people. Many patients don’t read them. Others think "it’s just a little painkillers."
What You Should Do Now
If you have heart failure:
- Check every medicine you take-prescription, over-the-counter, or herbal. Look for ibuprofen, naproxen, diclofenac, celecoxib, or ketoprofen.
- Switch to acetaminophen for pain relief. Stick to the lowest effective dose.
- Ask your doctor or pharmacist to review all your medications. Don’t assume they know you’re taking something from the pharmacy shelf.
- Track your weight daily. Report any gain over 1.5 kg in 24 hours.
- Teach a family member or caregiver how to spot early signs of fluid retention.
- Never take NSAIDs without talking to your heart failure specialist-even if you feel fine.
If you’ve already taken an NSAID and feel worse-swelling, weight gain, breathlessness-stop it immediately and call your doctor. Don’t wait. Don’t hope it passes. This isn’t a side effect you can tough out. It’s a medical emergency waiting to happen.
What’s Coming Next
Research continues. The PRECISION-ABPM trial is testing whether ultra-low NSAID doses might be safer, but early results from 2024 show almost no benefit. Meanwhile, the American College of Cardiology is developing a mobile app for heart failure patients that will alert them if they try to order or scan an NSAID at a pharmacy. It’s scheduled for release in mid-2025.
For now, the message hasn’t changed: avoid NSAIDs. Period. There’s no safe dose, no safe duration, no safe type. Your heart is already working too hard. Don’t make it work harder because you took a pill for a headache.
Can I take ibuprofen if I have heart failure?
No. Ibuprofen and all other NSAIDs increase the risk of fluid retention, high blood pressure, and heart failure hospitalization-even in small doses. There is no safe amount for people with heart failure. Use acetaminophen instead.
How quickly can NSAIDs cause heart failure symptoms?
Symptoms like swelling, weight gain, and shortness of breath can appear within 24 to 72 hours after taking an NSAID. A 2022 study showed the highest hospitalization risk occurs in the first week of use. Don’t wait for symptoms to get worse.
Is naproxen safer than ibuprofen for heart failure?
Some studies suggest naproxen may have a slightly lower cardiovascular risk compared to other NSAIDs, but it still causes fluid retention and worsens heart failure. No NSAID is considered safe. The difference in risk is small and not enough to justify use.
Can I take NSAIDs if I only use them once in a while?
Even occasional use increases your risk. A single dose can trigger fluid retention in vulnerable patients. The Danish study showed that exposure as short as 1-3 days significantly raised hospitalization rates. Avoid NSAIDs completely.
What should I do if I accidentally took an NSAID?
Stop taking it immediately. Monitor your weight daily and watch for swelling or shortness of breath. If you gain more than 1.5 kg in 24 hours or feel worse, contact your doctor or go to the emergency room. Don’t wait.
Are natural pain relievers safe for heart failure?
Not necessarily. Willow bark, ginger, and turmeric can have aspirin-like effects. Some herbal supplements interact with heart medications or affect kidney function. Always check with your doctor before trying anything new.
Why do some doctors still prescribe NSAIDs to heart failure patients?
Some doctors aren’t aware of the latest guidelines or assume the patient didn’t know the risk. Others may underestimate the danger of short-term use. But current guidelines from the American Heart Association and European Society of Cardiology are clear: NSAIDs are absolutely contraindicated. If your doctor prescribes one, ask why-and get a second opinion.





Deborah Andrich
11 December, 2025 . 17:24 PM
I knew someone who lost their independence because they took ibuprofen for a sprained wrist. They didn't even think it was a big deal. One week they were gardening, the next they were in the hospital with fluid in their lungs. This isn't just medical advice-it's life-saving info. If you have heart failure, treat NSAIDs like poison. No exceptions.
My mom's doctor never warned her either. She's 72, diabetic, and took Aleve for years. We only found out after she nearly died. Please, if you're reading this, check your cabinet right now.
Tommy Watson
13 December, 2025 . 04:14 AM
bro i took motrin for my back pain after my heart doc said i was good to go and i gained 8lbs in 2 days. i thought i was just fat from eating pizza but nope. ER visit. cath lab. they were like 'dude did you take ibuprofen?' i was like 'it was just two pills??' they looked at me like i just licked a live wire. i'm never touching that shit again. fuck NSAIDs. they're sneaky.
ps: my doctor still gives me prescriptions for it. like wtf??
Donna Hammond
14 December, 2025 . 10:47 AM
This is one of the most critical public health messages you'll ever read-and yet it's buried under layers of medical jargon and ignored by both patients and providers. Let me break it down plainly: NSAIDs don't just 'interfere' with heart failure-they actively sabotage your body's last-ditch efforts to survive. Your kidneys are already working overtime to keep your blood pressure up. Prostaglandins are your only ally. NSAIDs remove that ally. And then your heart, already damaged, is forced to pump against a tidal wave of fluid it can't handle.
Acetaminophen isn't perfect-it has liver risks-but it's the only painkiller that doesn't kill your kidneys while you're trying to save your heart. And yes, caregivers must audit medicine cabinets. Cold medicines? Check labels. Topical creams? Some contain diclofenac. Even 'natural' supplements like willow bark? They're aspirin in disguise.
This isn't fearmongering. It's epidemiology. The Danish study isn't an outlier-it's a pattern repeated across continents. If your doctor prescribes an NSAID to a heart failure patient, they're either misinformed or negligent. Demand a second opinion. Write it down. Show them this post. Save a life.
And if you're reading this and you're on NSAIDs? Stop today. Call your cardiologist tomorrow. Don't wait for swelling. Don't wait for breathlessness. Your body is screaming. Listen.
Sheldon Bird
15 December, 2025 . 23:46 PM
Thank you for this. Seriously. I'm a caregiver for my dad and we just found out he'd been taking naproxen for his arthritis for 3 years. He thought it was 'fine because it's OTC.' We switched him to Tylenol and he's been breathing easier since. I wish I'd known this sooner.
Also, I made a printable list of NSAIDs to avoid and posted it on the fridge. My dad says he forgets names but remembers 'the list.' Small wins, right? 😊
PS: If you're a nurse or pharmacist-please, please ask your patients about OTC meds. Don't assume they know.
Karen Mccullouch
16 December, 2025 . 11:00 AM
Who the hell lets Big Pharma get away with this? They knew. They knew for decades. They buried the studies. They let people die so they could sell more pills. And now they slap a tiny warning on the bottle like it's a 'maybe' and not a death sentence?
They don't care about you. They care about your prescription refill rate. If you're still using NSAIDs, you're being used. Wake up. This isn't medicine-it's corporate murder wrapped in a white pill.
And yeah, I'm mad. You should be too. 😡
nithin Kuntumadugu
17 December, 2025 . 01:46 AM
lol NSAIDs bad? yeah right. this is just the medical-industrial complex pushing acetaminophen because they own the patents. they dont want you using cheap pills that dont make them money. also i read somewhere that tylenol causes liver failure and its worse than ibuprofen. also my cousin in delhi takes diclofenac for 20 years and he still runs marathons. so maybe its just american fearmongering? 🤔
also i think the danish study was funded by pharma. its all a scam. dont trust the system. 🚩