Doctors prescribe generics every day - but how many truly understand why they’re just as safe and effective as brand-name drugs? Despite generics making up 90% of all prescriptions filled in the U.S., many physicians still hesitate. Not because they doubt the science, but because they’ve never been given clear, practical tools to explain it to patients - or to themselves.
Why Prescribers Still Doubt Generics
It’s not about distrust in the FDA. It’s about confusion. A 2023 survey of over 1,200 doctors found that nearly half couldn’t confidently explain what bioequivalence really means. They know generics are cheaper. But when a patient says, “My cousin took the generic version of Lipitor and felt worse,” how do you respond? The truth? Generics aren’t copies. They’re exact replicas in active ingredient, dosage, strength, and route of administration. The FDA requires them to deliver the same amount of drug into the bloodstream as the brand - within an 80% to 125% range. That’s not a loophole. That’s science. And it’s been proven in studies with 24 to 36 healthy volunteers for every single generic approved. Yet, 42% of Hispanic patients and 61% of physicians still worry about “authorized generics” - brand-name drugs sold under a generic label. That’s not fraud. It’s the same pill, just packaged differently. Without clear education, these nuances become myths.The FDA’s Prescriber Toolkit: What’s Actually Available
The U.S. Food and Drug Administration didn’t wait for doctors to ask for help. In 2022, they released Version 2 of their Prescriber Flyer - a single-page, printable guide designed to fit in any clinic waiting room. It includes QR codes linking to Spanish-language resources, because language barriers are part of the problem. But the real gem is the Generic Drugs Stakeholder Toolkit. It’s free. It’s updated. And it’s packed with tools you can use today:- Five customizable information cards you can hand to patients - no jargon, just facts.
- Three infographics, including one that visually breaks down how a generic tablet is made to match the brand in dissolution rate, absorption, and stability.
- Twelve ready-to-use social media templates for clinics to post on Facebook or Instagram.
What Other Organizations Are Doing
The American College of Physicians has been clear since 2015: “Prescribe generics whenever possible.” Their reasoning? Cost is the #1 reason patients stop taking their meds. One study showed 20-30% of new prescriptions are never filled because of price. Switching from a $300/month brand to a $37.50 generic doesn’t just save money - it saves lives. The CDC took a different angle. In their 2022 opioid prescribing guidelines, they pointed out that 78% of opioid prescriptions could be switched to generics without losing effectiveness. That’s not just a cost win - it’s a harm reduction strategy. In Europe, the EMA focuses more on dissolution profiles - how quickly the drug breaks down in the body - than on bioequivalence trials. It’s a slightly different path, but the end result is the same: safe, effective, cheaper drugs. The real gap? Integration. Only 37% of major electronic health record systems like Epic or Cerner show any pop-up or alert about generics when a doctor types in a brand name. That’s like having a GPS that never tells you the fastest route.
How Real Doctors Are Using These Resources
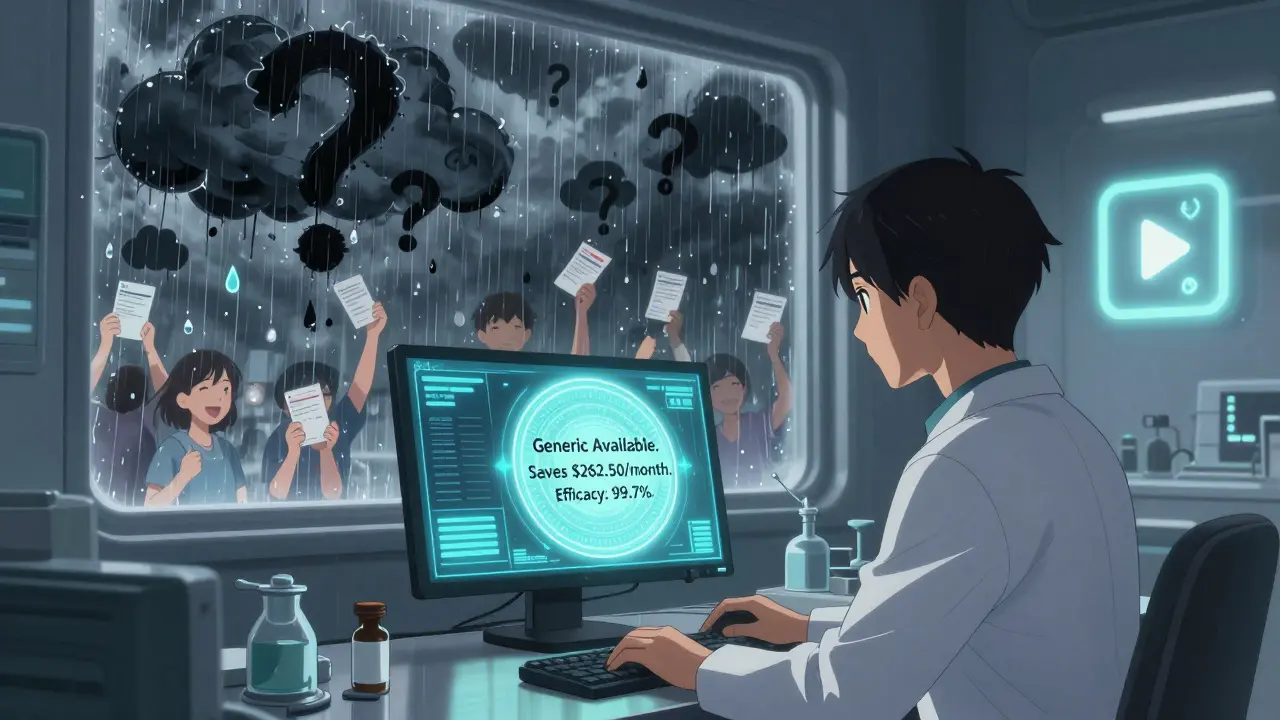
Dr. Sarah Chen, a family doctor in rural Nebraska, started using the FDA’s infographic in her office in 2021. Her generic prescribing rate jumped from 62% to 89% in 18 months. Why? Because her elderly patients - the ones most skeptical - saw the pictures. They saw the same FDA seal. They saw the same testing standards. But not everyone has that luxury. A 2022 study in the Annals of Internal Medicine found 73% of physicians said they simply don’t have time to dig through PDFs during a 10-minute visit. That’s why the most successful clinics embed the info directly into their EHRs. Kaiser Permanente did it in 2021. When a doctor tried to prescribe a brand-name statin, an alert popped up: “Generic available. Saves patient $262.50/month. Equivalent efficacy: 99.7%.” Within six months, brand prescribing dropped by 18.7%. One doctor on Reddit, @DrJenkins_MD, summed it up: “I need this info in my Epic alert box, not as a PDF I have to hunt for.”What Works in Practice: The Three-Step Plan
You don’t need a PhD in pharmacology to get better at prescribing generics. You just need a system. The CDC recommends this simple three-step approach:- 15-minute training - Watch the FDA’s 12-minute video on the ANDA process. No fluff. Just how generics get approved.
- Conversation prompts - Add a checkbox to your intake form: “Any concerns about switching to a generic?” Then have a script ready: “The FDA requires generics to work just like the brand. We’ve seen this work for thousands of patients like you.”
- Monthly feedback - Track your own prescribing rate. Compare it to your peers. Awareness changes behavior.
The Bigger Picture: Why This Matters
From 2010 to 2020, generics saved the U.S. healthcare system over $2.29 trillion. That’s not a number. That’s millions of people who kept their insulin, their blood pressure meds, their antidepressants - because they could afford them. By 2025, that number will hit $4.16 trillion in total savings. But only if doctors keep prescribing them. The FDA’s new API pilot - connecting generic data directly to EHRs - is the next step. In early trials, physicians using it increased generic prescribing by 15.2%. That’s not a trend. That’s a revolution. And it’s not just about money. It’s about equity. Patients earning under $25,000 a year are 3.7 times more likely to skip meds because of cost. When you prescribe a generic, you’re not just saving them cash. You’re giving them dignity.What’s Missing - And What You Can Do
The tools exist. The data is solid. The science is settled. What’s missing? Integration. Time. And confidence. Start small. Print one of the FDA’s information cards. Put it on your desk. Use it the next time a patient asks, “Is this the same?” Ask your clinic’s IT team if they can add a generic substitution alert to your EHR. If they say no, ask why. Then show them the Kaiser Permanente results. And if you’re still unsure? Watch the 12-minute FDA video. Read the Prescriber Flyer. Talk to your pharmacist. You’ll find the answers are simpler - and more powerful - than you thought.Frequently Asked Questions
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also deliver the same amount of drug into the bloodstream - within a scientifically accepted range of 80% to 125%. Over 24,000 adverse event reports analyzed in 2022 showed no difference in safety between brand and generic drugs.
Why do some patients feel worse after switching to a generic?
Most often, it’s not the drug - it’s the expectation. A 2023 study found patients who believed generics were inferior reported more side effects, even when taking the exact same medication. In rare cases, differences in inactive ingredients (like fillers or dyes) can cause minor reactions, but these are not therapeutic failures. For most drugs, including blood pressure meds, statins, and antidepressants, switching to a generic has zero impact on outcomes.
What’s the difference between a generic and an authorized generic?
An authorized generic is made by the original brand-name company but sold under a generic label - same pill, same factory, same packaging, just cheaper. It’s not a copy. It’s the exact same product. Confusion around this term is common, but it’s not a loophole - it’s a pricing strategy. The FDA confirms authorized generics meet all the same standards as other generics.
Why don’t my electronic health records suggest generics?
Only 37% of major EHR systems like Epic or Cerner currently include generic substitution alerts. That’s changing. The FDA launched an API pilot in 2023 that connects generic drug data directly to EHRs. Early results show a 15% increase in generic prescribing among participating clinics. Ask your IT department to check if your system supports FDA’s generic drug data feed.
Can I trust generics for complex drugs like inhalers or injectables?
For most complex drugs, yes - but the science is harder. Inhalers, topical creams, and some injectables require additional testing because delivery matters as much as the drug itself. The FDA has approved dozens of generic versions of these, but prescribers should review the specific approval details. Resources like the FDA’s Generic Drugs Stakeholder Toolkit include guidance for complex generics. If in doubt, consult your pharmacy or a clinical pharmacist.






Theo Newbold
21 December, 2025 . 20:26 PM
The FDA’s bioequivalence range of 80–125% is mathematically sound, but it’s not a magic bullet. When you’re dealing with narrow therapeutic index drugs like warfarin or levothyroxine, even minor variability in dissolution profiles can trigger clinical consequences. The data may say ‘no difference,’ but real-world pharmacovigilance tells a different story - especially in polypharmacy elderly patients. This isn’t skepticism. It’s harm reduction.
Orlando Marquez Jr
22 December, 2025 . 05:59 AM
The assertion that generics are ‘exact replicas’ is scientifically inaccurate. While active ingredients are identical, excipients vary across manufacturers and can influence bioavailability, particularly in patients with gastrointestinal disorders or allergies. The FDA’s standards ensure safety, but they do not guarantee therapeutic equivalence in all clinical contexts. Professional judgment remains indispensable.
Jon Paramore
23 December, 2025 . 00:28 AM
Let’s cut through the noise: ANDA pathway requires dissolution profile matching within ±10% of the innovator at three pH levels. That’s not ‘close enough’ - that’s bioequivalence by design. The 24–36 subject trials are powered for Cmax and AUC with 90% CI bounds. If you’re still doubting, you’re not reading the ANDA submissions - you’re reading anecdotes. The data is robust. The resistance is cultural.
Swapneel Mehta
23 December, 2025 . 00:45 AM
Really appreciate this breakdown. I’m from India, where generics are the norm, and it’s refreshing to see the science being shared so clearly. The infographic about manufacturing lines? Brilliant. We don’t have the luxury of brand loyalty here - but we do have trust in the system. Maybe the US just needs to see the same pictures.
Ben Warren
23 December, 2025 . 01:05 AM
It is deeply concerning that medical professionals are being encouraged to rely on marketing materials - however well-intentioned - rather than critical appraisal of pharmacokinetic literature. The FDA’s toolkit is not a substitute for clinical pharmacology training. To equate a printed infographic with evidence-based practice is not only irresponsible, it is a dangerous erosion of professional autonomy. The fact that 89% prescribing rates were achieved through visual aids, not education, is a failure of medical pedagogy, not a triumph.
Teya Derksen Friesen
24 December, 2025 . 20:09 PM
This is exactly the kind of clarity our system needs. I’ve been using the FDA’s patient cards in my clinic since last year - and my patients actually ask for generics now. Not because they were pressured, but because they finally understood. That’s not just prescribing. That’s patient empowerment. Keep pushing this.
Sandy Crux
26 December, 2025 . 10:36 AM
...and yet, the FDA still allows ‘authorized generics’ to be marketed as ‘generic’ - which, technically, they are not... they’re the original brand... under a different label... which means... the ‘generic’ label is misleading... and the entire narrative is built on semantic sleight-of-hand... and we’re supposed to believe this isn’t corporate manipulation...? ...and don’t even get me started on the ‘API pilot’... who’s funding that...? ...and why is Epic not integrating this...? ...and why are we not talking about the 15% increase being statistically insignificant in a population of 24,000...? ...and where’s the long-term data...? ...and why are we ignoring the 2018 Lancet meta-analysis on variability in generic anticonvulsants...? ...
Hannah Taylor
27 December, 2025 . 16:29 PM
lol generics are just the brand name drugs but with fake pills inside. my friend’s uncle took a generic adderall and his heart nearly exploded. the fda is in bed with big pharma. they don’t want you to know the real stuff is better. i got my rx from mexico and it’s way stronger. also, the coloring in generics gives you cancer. just saying.
Jason Silva
28 December, 2025 . 17:05 PM
Bro. I used to be skeptical too. Then I saw the FDA’s side-by-side dissolution test video. Same pill. Same factory. Same inspector. Just cheaper. 🤯 I started using the alert in my EHR - now I save my patients $200+ a month. No more ‘I can’t afford it.’ Just ‘I’m taking my meds.’ 🙌 If you’re still doubting, you’re not looking at the data - you’re listening to fear. Let’s fix this.
mukesh matav
29 December, 2025 . 12:59 PM
Thank you for sharing this. In my clinic, we use the 15-minute video during morning huddles. It takes less time than checking vitals. Patients respond better when they see the same FDA seal on the generic. Simple. Clear. Effective.