Night Shift Medication Errors: Why They Happen and How to Prevent Them
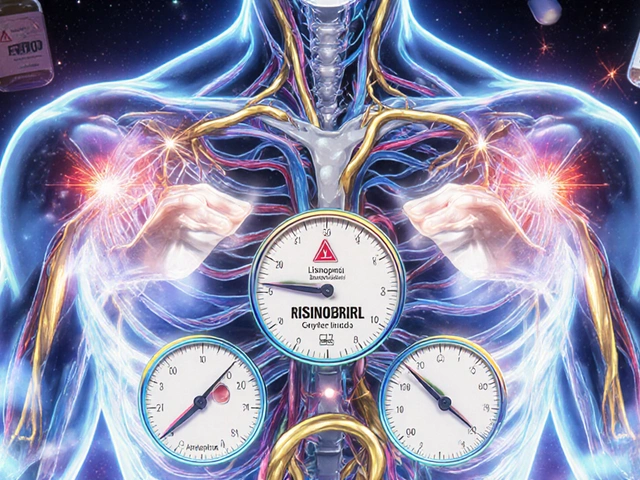
When you think of medication errors, you might picture a pharmacist handing over the wrong pill. But the real danger often happens in the quiet hours—night shift medication errors, mistakes made by healthcare workers during overnight shifts due to fatigue, poor communication, or disrupted routines. Also known as overnight prescribing errors, these aren’t just accidents—they’re systemic risks built into how hospitals and pharmacies run 24/7. Studies show that pharmacists and nurses working night shifts are up to 30% more likely to make dosing mistakes, especially when juggling multiple high-risk drugs like anticoagulants, insulin, or sedatives.
The problem isn’t just tired minds. It’s the communication breakdowns, the lack of clear handoffs between day and night teams. A nurse might miss a note that a patient’s blood thinner was changed at 3 p.m., or a pharmacist might overlook a drug interaction because the system auto-populates a default dose. Then there’s the drug interaction, how certain meds behave differently when taken at night. For example, levothyroxine taken with nighttime PPIs like omeprazole won’t absorb properly, and clopidogrel’s antiplatelet effect drops when paired with the wrong acid reducer. These aren’t theoretical risks—they’re documented in real cases where patients ended up with clots or uncontrolled thyroid levels because their meds were given at the wrong time, by the wrong person, in the wrong context.
It’s not just about people being sleepy. It’s about systems that assume night staff have the same resources, support, and clarity as day staff—and they don’t. No one’s asking for superheroes. They’re asking for better workflows: clear checklists, automated alerts for nighttime interactions, and enforced time buffers between dose checks. The medication safety, the process of preventing harm from drugs during administration you rely on during the day needs to be just as strong at 2 a.m.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll see how generic substitution laws can accidentally trigger errors when a night pharmacist swaps a brand drug for a generic without checking stability. You’ll learn why statins cause more muscle pain in women at night, and how antidepressants can lead to dangerous night sweats that mask overdose signs. There’s advice on using drug interaction checkers before midnight rounds, how to spot depression’s role in missed doses, and why expired meds in night cabinets are a ticking time bomb. These aren’t random posts—they’re all connected to the same root issue: night shift medication errors happen because we treat nighttime care like an afterthought. It’s time we stop doing that.
Medication Safety at Night: How Fatigue Increases Risk and What to Do About It
Night shift fatigue increases medication errors by up to 12.1%. Learn how sleep deprivation, sedating medications, and poor scheduling put patients at risk-and what you can do to stay safe.
View More