Urinary Tract Infection (UTI) Overview
When dealing with urinary tract infection, an infection that can affect any part of the urinary system, from kidneys to urethra. Also known as UTI, it typically shows up as painful or frequent urination, a burning sensation, and sometimes fever or back pain. The infection is usually sparked by a bacterial infection, most often Escherichia coli that travels from the gut to the urinary tract.
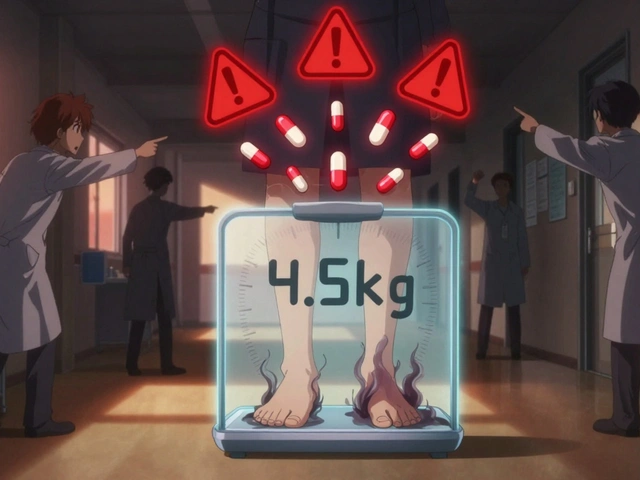
Doctors confirm a UTI with a urine test, a quick dip‑stick or lab analysis that checks for bacteria, white blood cells, and nitrites. Once confirmed, the mainstay of care is a short course of antibiotics, drugs that either kill the bacteria or stop them from multiplying. Common choices include trimethoprim‑sulfamethoxazole, nitrofurantoin, or fosfomycin, each selected based on local resistance patterns and patient factors. Drinking plenty of water, emptying the bladder frequently, and practicing good genital hygiene reduce the chance of recurrence. For people prone to frequent infections, doctors may recommend a low‑dose prophylactic antibiotic after sexual activity or at night.
Complications can arise if the infection spreads to the kidneys, leading to pyelonephritis – a more serious condition that demands prompt, often intravenous, antibiotic therapy. Certain groups, such as women, pregnant individuals, the elderly, and catheter users, face higher risks and may need tailored prevention strategies. Lifestyle tweaks like avoiding irritating soaps, wiping front‑to‑back, and staying hydrated are simple yet powerful. urinary tract infection knowledge empowers you to spot symptoms early, seek proper testing, and choose the right treatment. Below you’ll find a curated collection of articles that dive deeper into antibiotic comparisons, symptom management, and practical tips for staying infection‑free.
Nitrofurantoin, G6PD Deficiency & Hemolytic Anemia Risk - What You Need to Know
Learn why nitrofurantoin can cause hemolytic anemia in G6PD‑deficient patients, who’s at risk, and how to safely prescribe alternatives.
View More