Generic Substitution Laws: What You Can and Can't Be Forced to Accept
When a pharmacist hands you a different pill than what your doctor wrote on the script, it’s not a mistake—it’s generic substitution laws, state and federal rules that let pharmacies swap brand-name drugs for cheaper generic versions under certain conditions. Also known as drug substitution rules, these laws exist to cut costs, but they don’t always protect your health. Not all generics are equal, and some patients—especially those on psychiatric meds, thyroid drugs, or seizure treatments—can have serious problems when switched without warning.
These laws tie directly to pharmacy reimbursement models, how pharmacies get paid for dispensing generic drugs. Many insurers and pharmacy benefit managers (PBMs) push generics because they make more money off the spread between what they pay the pharmacy and what they charge you. But when a pharmacy gets paid more to switch you to a generic, your doctor’s original prescription can get overridden—even if you’ve been stable on the brand for years. That’s where patient rights, legal protections that let you refuse a substitution if it’s unsafe or ineffective come in. Some states require pharmacists to notify you before switching, others let them swap automatically unless your doctor writes "Do Not Substitute" on the script.
It’s not just about cost. A switch to a generic version of levothyroxine, for example, can throw off your thyroid levels and make you feel worse—even if the FDA says they’re "bioequivalent." The same goes for antidepressants and antiseizure drugs, where tiny differences in absorption can lead to relapse or side effects. That’s why brand medication, the original drug made by the company that developed it isn’t just a label—it’s sometimes your only stable treatment. And if you’re being pressured to switch, you’re not being difficult. You’re being smart.
These laws also connect to how pharmacies stay open. Many operate on razor-thin margins because of MAC pricing, the maximum allowable cost set by PBMs for generic drugs. When the MAC drops below what the pharmacy paid for the drug, they lose money on every prescription. That’s why they push generics—even when it’s not best for you. But you have tools: you can ask your doctor to write "Dispense As Written" or "Brand Necessary," you can appeal to your insurer, and in some states, you can even file a complaint if you’re switched without consent.
What you’ll find below are real stories and practical guides from people who’ve been through this. From how to talk to your doctor about staying on your brand drug, to understanding why biosimilars need special monitoring, to knowing exactly which laws protect you in 2025—these posts give you the facts you need to take control. No fluff. No jargon. Just what works when your health is on the line.
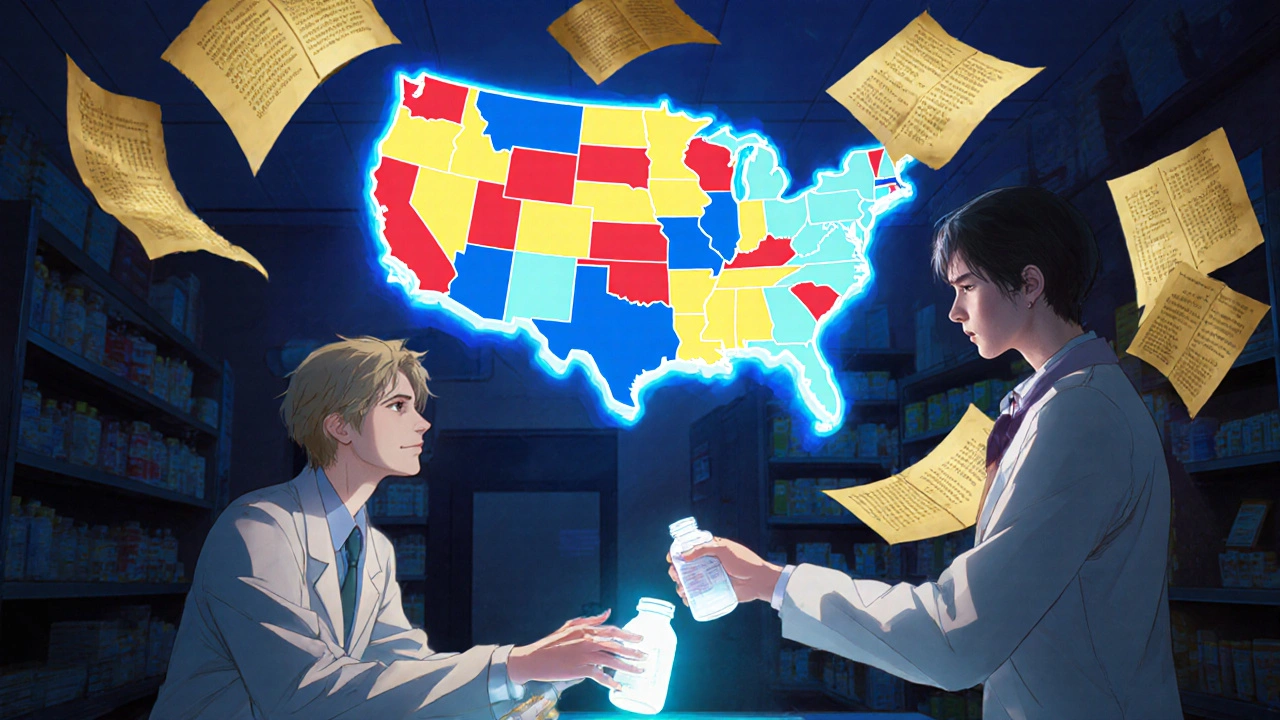
How Generic Substitution Laws Work: State-by-State Breakdown
Generic substitution laws vary widely across U.S. states, affecting how and when pharmacists can swap brand-name drugs for cheaper generics. Learn how each state regulates substitutions, who must give consent, and why some drugs are exempt.
View More